Understanding Myeloma: Challenges and Advances
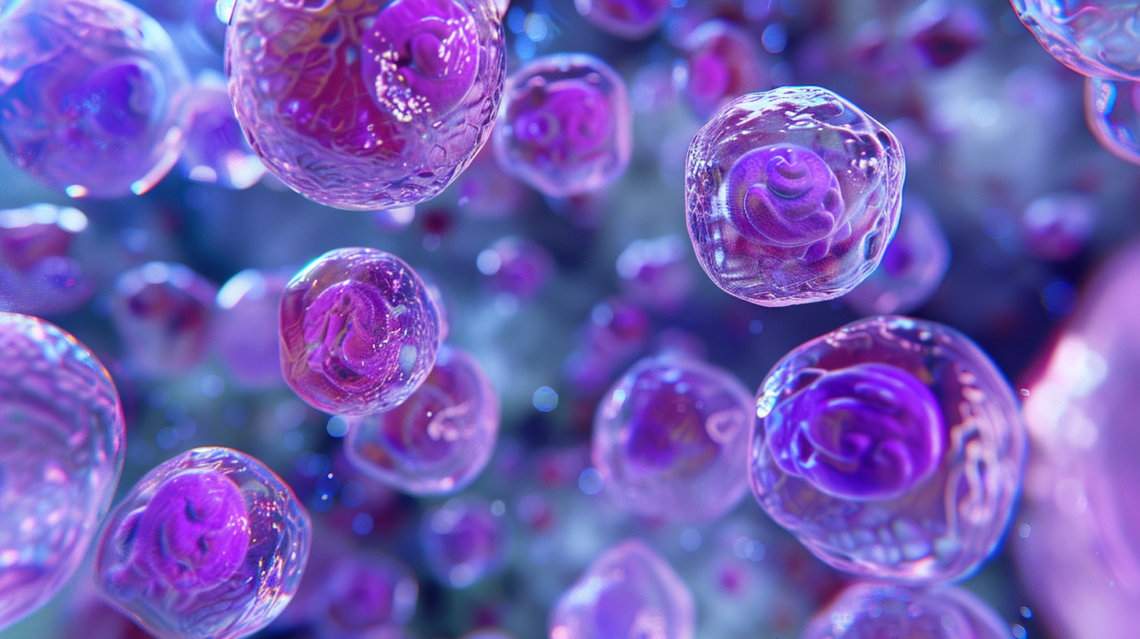
Myeloma, the second most prevalent type of blood cancer in Canada, remains a largely unknown entity to the broader public, a fact that underscores a disconcerting gap in the collective awareness of a disease that affects a significant number of individuals each year. This form of cancer is distinguished by the aberrant behavior and unchecked proliferation of a specific kind of white blood cell known as the plasma cell. Plasma cells, originating in the bone marrow—a soft, spongy tissue residing within the cavities of bones—are instrumental to the human immune system. They are tasked with the vital function of fighting infections through the production of antibodies that target and neutralize pathogens. However, in the context of myeloma, these cells undergo a malignant transformation, becoming what are referred to as myeloma cells. These cancerous cells disrupt the normal production of healthy blood cells within the bone marrow, marking the onset of a complex, multifaceted disease process.
One of the hallmark features of myeloma is its production of abnormal proteins, variously identified as monoclonal protein, monoclonal immunoglobulin, or M-protein, in lieu of the beneficial antibodies that combat infections. The presence of these abnormal proteins can lead to a host of serious complications, adversely affecting various organs and systems within the body, most notably the bones and kidneys. Occasionally, myeloma cells may aggregate, forming a mass known as a plasmacytoma—a tumor comprised of plasma cells—adding another layer of complexity to the disease’s pathology and its clinical management.
The etiological factors underlying myeloma are yet to be fully elucidated, though emerging research points to a potential interplay of decreased immune functionality, genetic predispositions, and environmental factors. The incidence of myeloma in Canada has been on a steady incline, presenting an ever-growing challenge to healthcare providers and researchers alike. Despite the absence of a cure, significant advancements in the field of medical research and the development of novel therapeutic strategies have markedly improved the outlook for those diagnosed with myeloma, enabling them to lead longer, more fulfilling lives.
In the disease’s early stages, individuals may exhibit no symptoms, with myeloma often being incidentally detected through routine blood tests. This asymptomatic phase complicates early detection efforts and underscores the insidious nature of myeloma. More commonly, however, individuals seek medical attention due to vague yet persistent symptoms such as back or bone pain, profound fatigue, or frequent infections—symptoms that are sometimes mistakenly attributed to aging. These clinical manifestations primarily arise from the excessive accumulation of plasma cells in the bone marrow and the presence of M-protein in the blood or urine, contributing to a range of complications that can significantly impair quality of life.
The management of myeloma is highly personalized, with treatment strategies being informed by an array of factors. These include the findings from physical exams and a suite of diagnostic tests (including blood, urine, and bone tests), the disease’s stage at diagnosis, prognostic indicators that help predict the disease course and treatment response, the patient’s age and overall health, the specific symptoms and disease complications experienced, and the patient’s response to any previous treatments. Additionally, the availability of new treatments through clinical trial participation offers hope for more effective management strategies and possibly curative therapies in the future.
The primary objectives of myeloma treatment encompass controlling the disease by inhibiting the production of abnormal plasma cells, strengthening bones to prevent fractures, increasing the red blood cell count to reduce fatigue, reducing the risk of infections, and overall promoting the patient’s well-being and quality of life. Achieving these goals requires a concerted effort from a multidisciplinary healthcare team, employing a combination of pharmacological treatments, supportive care, and, in some cases, innovative therapies under clinical trial protocols.
In recent years, the landscape of myeloma treatment has been revolutionized by the introduction of new drug classes, including proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies, which have significantly extended survival rates and improved the quality of life for patients. These therapeutic advances, coupled with better diagnostic tools and a deeper understanding of the disease’s molecular underpinnings, offer a glimmer of hope in the fight against myeloma. However, the journey from diagnosis to treatment is fraught with challenges, not least of which is the emotional and psychological toll on patients and their families. Navigating these challenges requires not only medical intervention but also comprehensive support services to address the myriad needs of those affected by this complex disease.
As research continues to unravel the mysteries of myeloma, it is imperative that awareness of the disease is heightened among the general public and healthcare professionals alike. Early detection and timely, tailored treatment are critical to improving outcomes for those diagnosed with myeloma. Furthermore, ongoing investment in research and development is essential to uncovering new therapeutic targets and ultimately, finding a cure for this formidable foe. In the meantime, the resilience and courage of those living with myeloma, together with the dedication of the medical community and the support of loved ones and advocacy groups, are pivotal in navigating the challenges posed by this disease. The journey of myeloma, from its diagnosis to the management and beyond, encapsulates not just the struggles encountered in the face of a chronic condition but also the triumphs of human spirit, scientific inquiry, and collaborative care.
The progression of myeloma treatment and care underscores a broader narrative within the medical community—one of relentless pursuit of knowledge and the continuous improvement of therapeutic modalities. This journey is marked by the translation of research findings into clinical practice, the adaptation of treatment protocols to reflect the latest evidence, and the personalized approach to care that considers the unique circumstances of each patient. As such, the management of myeloma is a testament to the advancements in precision medicine, where genetic and molecular profiling of tumors informs treatment decisions, promising a more targeted and effective approach to combating the disease.
Yet, the battle against myeloma extends beyond the confines of clinics and research laboratories. It is a collective effort that necessitates robust support systems to address the physical, emotional, and financial burdens of the disease. Support groups, patient advocacy organizations, and online communities play an invaluable role in providing a platform for sharing experiences, offering emotional support, and disseminating information about the latest research developments and clinical trials. These networks not only empower patients and their families but also foster a sense of community and solidarity in the face of adversity.
Moreover, the increasing prevalence of myeloma in Canada and globally highlights the need for heightened awareness and education about the disease among the public and healthcare providers. Early detection and awareness of symptoms can lead to timely diagnosis and treatment, potentially improving outcomes. Public health campaigns, educational seminars, and awareness events are instrumental in elevating the visibility of myeloma and encouraging individuals to seek medical advice for persistent, unexplained symptoms.
The evolution of myeloma treatment also underscores the importance of clinical trials in advancing medical knowledge and improving patient care. Clinical trials offer patients access to cutting-edge therapies and the opportunity to contribute to scientific discovery that can benefit future generations. However, the decision to participate in a clinical trial is complex and requires careful consideration of the potential risks and benefits, underscoring the need for transparent communication and shared decision-making between patients and their healthcare providers.
The journey of myeloma, from its elusive beginnings to the complex challenges of its management, is a narrative of resilience, innovation, and hope. While the path to a cure remains arduous, the advancements in research, treatment, and patient care offer a beacon of hope for those affected by this disease. As we continue to unravel the mysteries of myeloma, the collective efforts of the medical community, patients, families, and advocacy groups will remain instrumental in improving outcomes and quality of life for those on this journey. In the face of myeloma, it is this spirit of collaboration, perseverance, and compassion that defines our path forward, promising a future where myeloma can be effectively managed or, perhaps one day, cured.

