Enteropathic Arthritis
Enteropathic arthritis, a form of chronic, inflammatory arthritis associated with inflammatory bowel disease (IBD), affects a significant portion of individuals dealing with conditions like Crohn’s disease and ulcerative colitis. This article aims to provide a comprehensive understanding of enteropathic arthritis, delving into its causes, symptoms, diagnosis, and treatment strategies, with a focus on Canadian healthcare perspectives.
Understanding Enteropathic Arthritis
A. Definition and Association with IBD
Enteropathic arthritis falls under the umbrella of spondyloarthritis, a group of inflammatory rheumatic diseases. It primarily affects the joints, but its connection to IBD indicates a complex interplay between the gut and the immune system.
B. Prevalence
Statistics from Canadian healthcare databases suggest that a notable percentage of IBD patients experience enteropathic arthritis, with varying severity and joint involvement.
Causes and Pathophysiology
A. The Gut-Joint Axis
The exact cause of enteropathic arthritis remains a subject of ongoing research. The prevailing theory suggests an autoimmune component, where the body’s immune response, initially targeted at the gut, extends to the joints.
B. Genetic and Environmental Factors
Genetic predispositions, coupled with environmental triggers, play a crucial role. Certain genetic markers, like HLA-B27, are frequently associated with a higher risk of developing spondyloarthritis.
Clinical Presentation
A. Symptoms
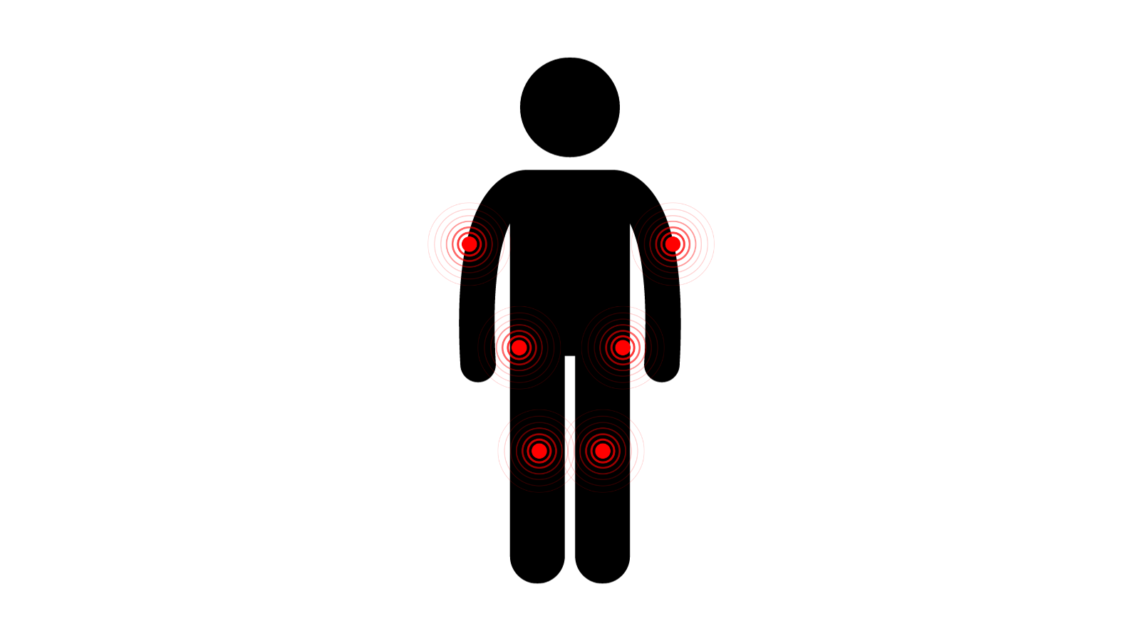
Patients with enteropathic arthritis commonly report:
- Joint pain and swelling, predominantly in the lower limbs.
- Stiffness, especially in the morning.
- In severe cases, the spine and sacroiliac joints are affected, leading to back pain and reduced mobility.
B. Association with IBD Flare-ups
Symptoms of enteropathic arthritis often correlate with the activity of bowel disease, but joint symptoms can precede, follow, or occur independently of intestinal symptoms.
Diagnosis
A. Diagnostic Challenges
Diagnosing enteropathic arthritis involves distinguishing it from other forms of arthritis, which can be challenging due to overlapping symptoms with rheumatoid arthritis and osteoarthritis.
B. Diagnostic Tools
A combination of medical history, physical examination, blood tests (like ESR and CRP for inflammation), imaging techniques (X-rays, MRI), and consultation with rheumatologists forms the core of the diagnostic process.
Treatment and Management
A. Multidisciplinary Approach
Treatment often involves a team of specialists, including gastroenterologists, rheumatologists, and physical therapists. Management strategies are tailored to individual patient needs, taking into account the severity of both joint and bowel symptoms.
B. Medications
- Nonsteroidal anti-inflammatory drugs (NSAIDs) provide symptomatic relief.
- Disease-modifying antirheumatic drugs (DMARDs), like sulfasalazine and methotrexate, are used for more severe cases.
- Biologic therapies targeting specific immune system components have shown promise, particularly TNF inhibitors.
C. Lifestyle Modifications
In addition to medications, lifestyle changes, such as regular exercise, a balanced diet, and smoking cessation, are crucial in managing symptoms and improving overall quality of life.
D. Surgical Interventions
In rare cases where joint damage is severe, surgical interventions may be considered.
Prognosis
The prognosis of enteropathic arthritis varies. While some individuals experience mild, episodic symptoms, others might face chronic, debilitating pain. Early diagnosis and effective management are key to improving long-term outcomes.
Enteropathic arthritis, as a complex interplay between the gut and the immune system, presents unique challenges in both diagnosis and treatment. Understanding its intricacies is essential for providing comprehensive care to those affected. Continuous research and a multidisciplinary approach remain critical in improving the quality of life for patients with this condition. As always, Canadian healthcare providers are dedicated to staying at the forefront of managing such intricate medical conditions, ensuring patients receive the best possible care based on current medical evidence and practices.

