Lymphedema
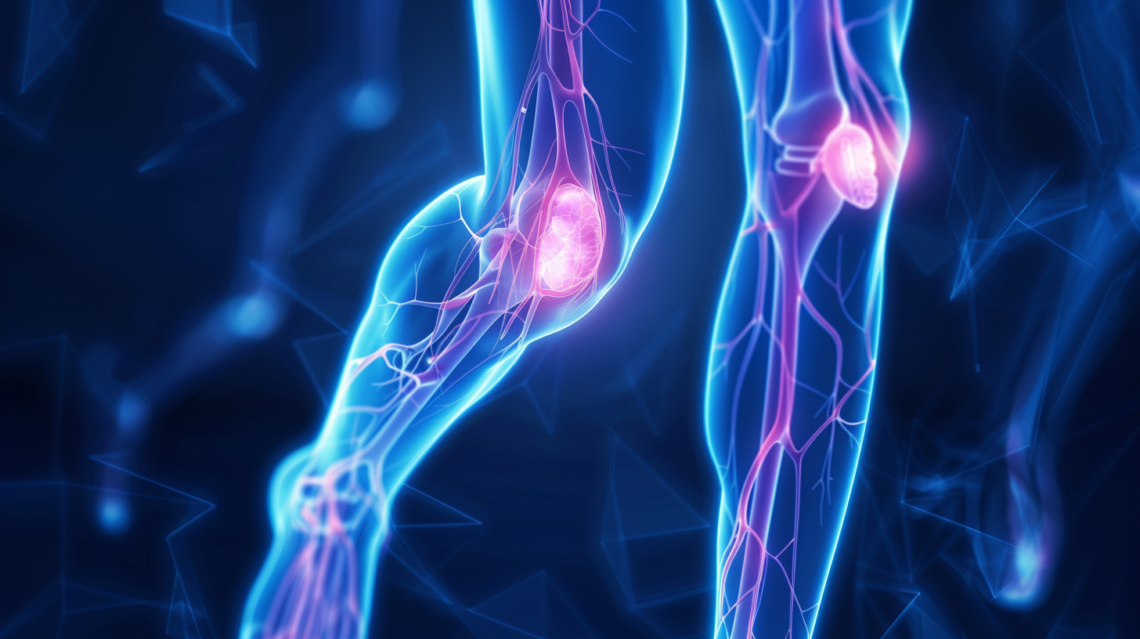
Lymphedema stands as a significant health concern, characterized by the swelling that results from the accumulation of lymphatic fluid in the body’s tissues—a manifestation of the lymphatic system’s failure to adequately drain this fluid. This system, essential to both the immune and circulatory systems, functions not only to transport lymph, a fluid replete with white blood cells and waste products, back to the bloodstream but also plays a pivotal role in defending the body against infections and diseases. When the lymphatic system is compromised—whether through damage or malformation—lymph fluid builds up, leading to the swelling indicative of lymphedema. Predominantly affecting the limbs, although it can also occur in the chest, abdomen, and genital areas, lymphedema can have profound impacts on an individual’s physical and emotional well-being.
Lymphedema is most frequently associated with individuals who have undergone treatment for cancer, especially when these treatments involve the removal or radiation of lymph nodes, which are critical components of the lymphatic system. This association underscores the dual burden faced by cancer survivors, who, in addition to overcoming cancer, may find themselves grappling with the long-term consequences of their treatment. Notably, the risk of developing lymphedema is not confined to the immediate aftermath of treatment but persists throughout a survivor’s lifetime, adding a layer of complexity to post-cancer care and surveillance.
The symptomatology of lymphedema extends beyond the visible swelling, incorporating sensations of heaviness or tightness, reduced flexibility in the affected limbs, recurrent infections, and significant changes in the texture and quality of the skin. These symptoms, which can range from mild to severely debilitating, underscore the importance of early diagnosis and intervention. Indeed, early-stage lymphedema may be managed more effectively, preventing the progression to more advanced stages, which are characterized by irreversible skin changes and increased vulnerability to infections.
The risk factors for lymphedema are multifaceted, encompassing not only medical treatments like surgery and radiation therapy but also lifestyle and genetic factors. Obesity, for instance, significantly increases the risk of lymphedema, as the excess body weight exerts additional pressure on the lymphatic system. Similarly, inflammatory conditions such as rheumatoid arthritis or infections that impair lymphatic flow can precipitate the onset of lymphedema. Genetic predispositions to inadequate lymphatic structures further complicate the risk landscape, illustrating the complex interplay of factors that contribute to this condition.
Managing lymphedema requires a comprehensive and multidisciplinary approach, tailored to the individual’s specific circumstances and needs. Compression therapy, one of the cornerstones of lymphedema management, involves the use of specially designed garments to support and enhance lymphatic drainage. Manual lymphatic drainage, a form of gentle massage that encourages the movement of lymph fluid out of the affected tissues, offers another therapeutic option, often in conjunction with physical exercises designed to stimulate lymphatic flow. For individuals with more advanced or refractory lymphedema, surgical options may be explored, though these are generally considered only after conservative measures have been exhausted.

