Diseases and Disorders
-
Crohn’s and Colitis
Crohn’s disease and colitis, often grouped under the umbrella term ‘inflammatory bowel diseases’ (IBD), represent a significant challenge in the field of gastroenterology. Despite their prevalence and impact, misconceptions and uncertainties about these conditions persist. This article aims to demystify Crohn’s and colitis, delving into their pathophysiology, symptoms, diagnosis, treatment, and the lived experiences of those affected.
At the core, Crohn’s disease and Colitis are chronic conditions characterized by inflammation of the gastrointestinal (GI) tract. However, they exhibit distinct patterns of inflammation and affected areas. Crohn’s disease can affect any part of the GI tract, from mouth to anus, but commonly targets the end of the small intestine and the beginning of the colon. Colitis, specifically ulcerative colitis, is confined to the colon and the rectum. The inflammation in Crohn’s disease tends to be patchy and transmural, affecting the entire thickness of the bowel wall. In contrast, colitis usually involves continuous inflammation of the innermost lining of the colon. These differences in inflammation patterns not only help in distinguishing the two but also influence their symptomatology and complications.
Symptoms and Diagnosis: A Multifaceted Challenge
Both Crohn’s and colitis manifest with a spectrum of symptoms, often overlapping yet distinct in their presentation. Common symptoms include persistent diarrhea, abdominal pain, rectal bleeding, weight loss, and fatigue. Crohn’s disease may also lead to complications such as strictures, fistulas, and abscesses, owing to its transmural inflammation. Colitis, in severe cases, can result in toxic megacolon, a life-threatening complication.
Diagnosing these conditions involves a comprehensive approach. A detailed medical history and physical examination are paramount. Diagnostic tools include blood tests, stool tests, endoscopic procedures like colonoscopy, and imaging studies such as MRI or CT scans. Biopsies taken during endoscopy can be pivotal in confirming the diagnosis and assessing the extent and severity of inflammation.
The Etiological Puzzle: Genetics and Environment
The exact cause of Crohn’s disease and colitis remains elusive, but it is widely acknowledged that a combination of genetic, environmental, and immune factors plays a role. Genetic predisposition is evident, with a higher incidence in individuals with a family history of IBD. Environmental factors, including diet, lifestyle, and exposure to certain microbes, are also believed to contribute to the onset and progression of these diseases.
Treatment Modalities: Tailoring to Individual Needs
Treatment for Crohn’s and colitis is multifaceted and tailored to the severity and location of the disease. The primary goal is to reduce inflammation, manage symptoms, and prevent complications. Medications form the cornerstone of treatment, including aminosalicylates, corticosteroids, immunomodulators, and biologic therapies. These drugs help control inflammation and induce and maintain remission. In cases where medication is ineffective, surgery may be necessary. For Crohn’s disease, this could involve resection of the affected bowel segment, while colitis may require a colectomy in severe cases. It’s crucial to understand that surgery is not a cure but a means to manage complications and improve quality of life.
Living with Crohn’s and Colitis: A Holistic Perspective
Living with Crohn’s or colitis goes beyond managing physical symptoms. These conditions can have profound psychosocial impacts, affecting mental health, personal relationships, and quality of life. Patients often grapple with the unpredictability of flare-ups and the chronic nature of their illness. Comprehensive care, therefore, includes not only medical treatment but also psychological support and lifestyle modifications. Dietary adjustments can help manage symptoms, and stress reduction techniques can be beneficial. Patient education and support groups play a vital role in empowering individuals to cope with their condition.
The Road Ahead: Research and Hope
Research continues to advance our understanding of Crohn’s disease and colitis. Emerging therapies, including newer biologics and stem cell treatments, offer hope for more effective and personalized management. Moreover, ongoing studies into the genetic and environmental aspects of these diseases promise to unravel more of their mysteries.
In conclusion, Crohn’s disease and colitis, as complex and challenging as they are, can be managed effectively with a comprehensive and personalized approach. Understanding these conditions, their impact, and the advancements in their management can empower patients and healthcare professionals alike in navigating these often turbulent waters of inflammatory bowel diseases.
-
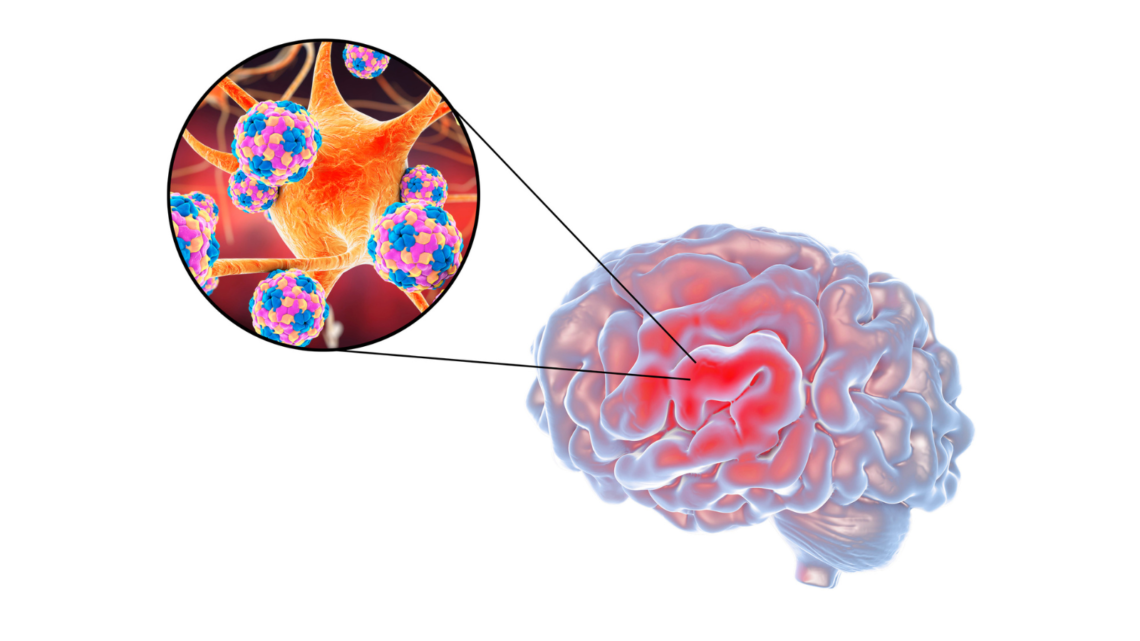
Meningitis Risks, Signs, and Prevention
Meningitis is a serious and often life-altering infection that has the potential to strike anyone, anywhere, and at any time, regardless of age or location. This illness, which affects the membranes surrounding the brain and spinal cord, can lead to an array of severe symptoms and complications that highlight its devastating nature. Affecting over 2.5 million people worldwide each year, meningitis leaves a powerful impact on individuals and families alike, with fatal outcomes in approximately one out of every ten cases. The impact is especially heartbreaking in children under five, who account for nearly half of all meningitis-related deaths worldwide. Surviving meningitis often comes with its own challenges, as roughly one in five survivors live with long-term disabilities, such as hearing loss, brain damage, epilepsy, and even the need for limb amputation. Given the significant impact and the indiscriminate nature of this infection, understanding the symptoms, risk factors, and treatment options is essential for both awareness and prevention.
The symptoms of meningitis, while often mistaken for other ailments in the early stages, can progress rapidly, especially in individuals over the age of two. Common signs include a sudden high fever and stiffness in the neck, accompanied by a severe headache. Other indications might involve nausea, vomiting, and in some cases, confusion or difficulty concentrating. As the infection progresses, seizures, drowsiness, and heightened sensitivity to light can also arise, while appetite loss and, in certain cases like meningococcal meningitis, a skin rash may occur. Recognizing these symptoms is crucial, as early intervention can significantly improve outcomes, especially for bacterial meningitis, which is notably the most severe form of the illness.
In infants and newborns, meningitis symptoms can present differently, adding an additional layer of complexity for concerned parents and caregivers. High fever, continuous crying, and pronounced irritability are some of the first signs. An infected infant may also become notably sleepy, difficult to wake, or display sluggishness or inactivity. Additional signs may include a reluctance to eat or wake for feeding, poor feeding habits, vomiting, and, in some cases, a visible bulge in the soft spot atop the baby’s head. Newborns may also develop stiffness in their neck and body, and in many cases, attempts to console the child may only lead to more intense crying, particularly when the infant is held. This variation in symptoms across age groups underscores the need for parents and caregivers to be vigilant and to seek prompt medical advice when these symptoms appear.
Meningitis can be caused by several infectious agents, including viruses, bacteria, fungi, and parasites. While viral meningitis is the most common and often resolves with minimal medical intervention, bacterial meningitis presents a much more severe threat. Left untreated, bacterial meningitis can lead to death within a matter of days, and delayed treatment increases the likelihood of lasting brain damage. Unlike viral cases, bacterial meningitis demands immediate antibiotic treatment, making early diagnosis and intervention vital to prevent life-threatening complications. While some forms of meningitis improve with limited treatment, others require urgent medical intervention to prevent a rapid escalation of symptoms and potentially fatal outcomes.
Immediate medical care is imperative if there is any suspicion of meningitis, whether it is a family member, friend, or oneself. Early treatment, particularly for bacterial meningitis, can avert many of the infection’s most serious complications and reduce the chance of long-term effects.
-
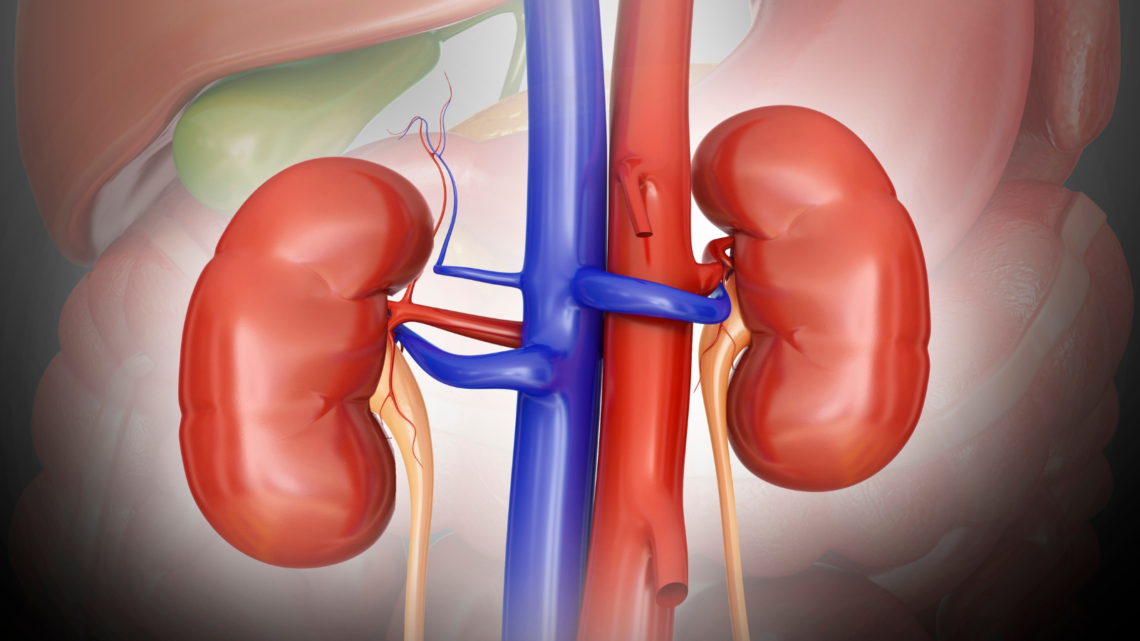
Kidney Disease
The number of Canadians living with kidney disease has been steadily increasing over the years. Currently, an estimated 1 in every 10 Canadians have kidney disease, while it affects as many as 850 million people worldwide. The kidneys are responsible for filtering excess water and waste from your blood and converting it to urine. They’re also responsible for balancing salt and minerals in your body, including calcium, sodium, potassium, and phosphorus, in addition to creating red blood cells, controlling blood pressure, and strengthening bones. However, when you have kidney disease, this means that your kidneys cannot properly filter blood in the way it should be. Over time, this can lead to kidney failure.
Because kidney disease can progress silently, early detection is key for being able to make the appropriate changes necessary in order to improve the health and function of your kidneys. There two main ways that kidney disease can be diagnosed: Through a blood test, or by urinalysis. A blood test will measure your level of serum creatinine, which will indicate how well your kidneys are (or how well they aren’t) functioning and filtering blood. During a urinalysis, labs techs will look for a protein known as albumin in your urine. If this protein is present, then there is a strong likelihood that your kidneys have some damage. The higher the albumin level is, the higher your risk is of losing function of your kidneys. Kidney disease can also be detected through biopsies, ultrasounds, and X-rays.
As for how you can prevent kidney disease from developing, it’s important that you have your blood pressure checked on a regular basis. If you have high blood pressure, this can speed up kidney disease – particularly if your high blood pressure is uncontrolled. Some medications have also been known to contribute to kidney disease, like over-the-counter painkillers such as NSAIDs. If you are going to be taking an over-the-counter medication, you should first double check with your physician or pharmacist to make sure it’s safe.
As mentioned, kidney disease is often a silently progressing disease, meaning symptoms will not always be present until it has reached a later stage. However, there are some symptoms that one can develop that may be an indicator of kidney disease and kidney failure. You may feel fatigued or find that you’re sleeping for an extended amount of time, you may feel cold, faint, dizzy or weak, your skin may feel itchy, you might have shortness of breath, have trouble concentrating or thinking clearly, have a swollen, puffy face or swelling of the hands or feet, upset stomach, nausea, vomiting, discoloured urine, have blood in your urine (which is one of the signs of kidney failure), or have difficulty passing urine.
Once you have received a definitive diagnosis of kidney disease, treatment is often geared towards treating the associated symptoms and any complications that can develop as a result of having kidney disease. For example, you may be prescribed medication to control high blood pressure or medication to lower cholesterol, medication to treat anemia, medical to treat swelling, as well as calcium D supplements to help protect and keep your bones strong.
If you develop kidney failure, you will most likely have to receive kidney dialysis, which is something that will artificially remove fluid and excess waste products from your blood when your kidneys are no longer able to do this on their own. In some cases, you may also require a kidney transplant. If you do undergo a kidney transplant, you will need to take medication to prevent your body from rejecting the new organ. In terms of diet, there are also certain things that you should avoid with kidney disease. For example, you should limit your intake of protein, as the more protein you eat, the harder it can be on weak kidneys. Foods that are high in potassium, such as nuts, avocados, mangos, bananas, oranges, spinach, tomatoes and potatoes, should also be avoided, as when you have kidney disease it can cause potassium to buildup in your body to levels that are considered unsafe. You also need to limit phosphorus, as well as your intake of salt, sugar, and starches. Canned foods and whole wheat bread should also be avoided. As for the types of foods that are considered safe to eat with kidney disease, some include apples, cranberries, blueberries, raspberries, strawberries, cherries, egg whites, onions, cabbage, cauliflower, and garlic.
-
Inflammatory Bowel Disease in Canada
Canada has one of the highest case rates of inflammatory bowel disease (IBD) in the world. A staggering 1 in 140 Canadians are living with some form of IBD, whether it be Crohn’s disease or ulcerative colitis. This translates to approximately 300,000 Canadians currently managing the daily challenges posed by these chronic conditions. Alarmingly, the number of Canadians with IBD is expected to rise to 400,000, roughly 1% of the population, by 2030.
Understanding Inflammatory Bowel Disease
Inflammatory bowel disease is an umbrella term used to describe disorders that involve chronic inflammation of the digestive tract. The two main types of IBD are Crohn’s disease and ulcerative colitis. While both conditions cause inflammation of the digestive tract, they affect different parts and have some distinct characteristics.
Crohn’s disease can occur anywhere along the gastrointestinal tract from the mouth to the anus but most commonly affects the end of the small intestine (the ileum) and the beginning of the colon. The inflammation caused by Crohn’s disease often spreads deep into the layers of affected bowel tissue, which can lead to severe complications.
Ulcerative colitis, on the other hand, is limited to the colon and rectum. The inflammation in ulcerative colitis is usually confined to the innermost lining of the colon, whereas in Crohn’s disease, it can affect all layers of the bowel wall. Despite these differences, both conditions are marked by periods of active disease (flare-ups) and periods of remission.
Symptoms of IBD
IBD can manifest in a variety of symptoms that can be debilitating and significantly impact the quality of life. These symptoms can vary in severity and frequency and may include:
- Persistent diarrhoea
- Abdominal pain and cramping
- Blood in the stool
- Reduced appetite
- Unintended weight loss
- Fatigue
- Fever
The Aging Population and IBD
One of the most concerning trends in Canada is the increasing incidence of IBD among seniors. Individuals aged 65 and over with Crohn’s disease or ulcerative colitis represent the fastest growing demographic of Canadians with IBD. This shift presents unique challenges, as older adults often have other health issues that complicate the management of IBD, requiring more comprehensive and coordinated care.
The reasons behind this increase in IBD cases among seniors are not entirely clear. It is possible that improvements in diagnostic techniques have led to more cases being identified. Additionally, people with IBD are living longer due to advancements in medical treatments, resulting in a larger elderly population with the condition. Whatever the cause, the aging population with IBD poses significant challenges for the healthcare system.
Older adults with IBD may experience more severe symptoms and complications compared to younger individuals. They are also more likely to have other chronic conditions, such as heart disease, diabetes, or arthritis, which can complicate their treatment and care. The presence of multiple health issues can make it more difficult to manage IBD, as treatments for one condition may worsen another. Therefore, healthcare providers must take a holistic approach to care for older adults with IBD, considering all of their health needs.
Rural Disparities in Care
Geographical disparities play a significant role in the management of IBD in Canada. Canadians living in rural or remote areas who suffer from Crohn’s or colitis are less likely to receive care from gastroenterologists, who are specialists in these diseases. This lack of access to specialized care can lead to worse health outcomes, including increased disease complications and more frequent hospitalizations.
Rural patients face several challenges in accessing healthcare. These include long travel distances to reach healthcare facilities, limited availability of specialists, and fewer healthcare resources overall. As a result, rural patients with IBD may not receive timely and appropriate care, which can lead to disease progression and complications.
To address these disparities, it is crucial to improve access to specialist care and healthcare resources in rural areas. Telemedicine, which involves the use of telecommunications technology to provide healthcare services remotely, is one potential solution. Telemedicine can help bridge the gap in access to care by allowing rural patients to consult with specialists without having to travel long distances. Additionally, increasing the number of healthcare providers trained in IBD care and improving healthcare infrastructure in rural areas can help ensure that all Canadians with IBD receive the care they need.
The Impact on Children
IBD is not only a concern for adults; it significantly affects children as well. Over 7,000 Canadian children under the age of 18 live with Crohn’s disease or ulcerative colitis. The prevalence of these conditions in Canadian children has alarmingly increased by more than 50% in the past 15 years. This upward trend highlights the urgent need for continued research into the causes and treatments of IBD, as well as robust support systems for affected families.
Children with IBD face unique challenges compared to adults. The disease can impact their growth and development, as well as their ability to attend school and participate in normal childhood activities. The symptoms of IBD, such as abdominal pain and fatigue, can be particularly disruptive for children, affecting their quality of life and mental health.
In addition to the physical symptoms, children with IBD may also experience emotional and social challenges. They may feel isolated or different from their peers due to their condition, which can lead to anxiety and depression. It is essential to provide comprehensive care that addresses both the physical and emotional needs of children with IBD. This includes access to pediatric gastroenterologists, mental health support, and educational resources to help children and their families manage the disease.
The Role of Research and Innovation
Research and innovation play a crucial role in improving the understanding, diagnosis, and treatment of IBD. Ongoing research efforts aim to uncover the underlying causes of IBD, which are currently not well understood. It is believed that a combination of genetic, environmental, and immune system factors contribute to the development of IBD. By identifying these factors, researchers hope to develop more effective treatments and ultimately find a cure for IBD.
One area of research focuses on the role of the microbiome in IBD. The microbiome is the collection of microorganisms that live in the human gut, and it plays a crucial role in digestion and immune function. Studies have shown that individuals with IBD have an altered gut microbiome compared to healthy individuals. By understanding how the microbiome contributes to IBD, researchers may be able to develop treatments that restore a healthy balance of gut bacteria.
Another area of research involves the development of new medications and therapies for IBD. Traditional treatments for IBD include anti-inflammatory drugs, immune system suppressors, and surgery. While these treatments can be effective, they often come with significant side effects and may not work for all patients. Newer treatments, such as biologics and small molecule drugs, target specific pathways involved in the inflammatory process and offer more targeted and effective options for patients.
The Importance of Support Systems
Living with IBD can be incredibly challenging, both physically and emotionally. It is essential for individuals with IBD to have strong support systems in place to help them manage the disease and maintain their quality of life. Support can come from a variety of sources, including healthcare providers, family and friends, and patient advocacy organizations.
Healthcare providers play a crucial role in supporting individuals with IBD. They can provide education about the disease, develop treatment plans tailored to the individual’s needs, and offer emotional support. Regular follow-up appointments with healthcare providers are essential for monitoring the disease and adjusting treatment as needed.
Family and friends can also provide invaluable support to individuals with IBD. Understanding the challenges that come with the disease and offering emotional and practical support can make a significant difference in the lives of those affected. Simple acts of kindness, such as accompanying a loved one to a medical appointment or helping with daily tasks, can help alleviate some of the burdens associated with IBD.
Patient advocacy organizations, such as Crohn’s and Colitis Canada, provide resources, support, and advocacy for individuals with IBD and their families. These organizations offer educational materials, support groups, and opportunities for individuals to connect with others who are going through similar experiences. They also advocate for policies and initiatives that improve the lives of those with IBD, such as increased funding for research and improved access to healthcare.
The Role of Diet and Nutrition in Managing IBD
Diet and nutrition play a critical role in managing IBD. While there is no specific diet that can cure IBD, certain dietary changes can help manage symptoms and improve overall health. It is important for individuals with IBD to work with a registered dietitian or healthcare provider to develop a personalized nutrition plan that meets their specific needs.
General Dietary Guidelines for IBD:
- Eat small, frequent meals: Eating smaller, more frequent meals can help reduce the burden on the digestive system and manage symptoms such as bloating and abdominal pain.
- Stay hydrated: It is important to drink plenty of fluids to prevent dehydration, especially during flare-ups when diarrhoea is more common.
- Avoid trigger foods: Certain foods can trigger symptoms in individuals with IBD. Common trigger foods include high-fat foods, spicy foods, caffeine, and alcohol. Identifying and avoiding these trigger foods can help manage symptoms.
- Focus on nutrient-dense foods: Individuals with IBD may have difficulty absorbing nutrients due to inflammation in the digestive tract. Eating a diet rich in nutrient-dense foods, such as fruits, vegetables, lean proteins, and whole grains, can help ensure adequate nutrition.
Specialized Diets for IBD:
Some individuals with IBD may benefit from specialized diets designed to reduce inflammation and manage symptoms. It is important to note that these diets should be followed under the guidance of a healthcare provider or registered dietitian.
- Low-FODMAP Diet: The low-FODMAP diet involves reducing the intake of fermentable carbohydrates, which can cause bloating and gas. This diet may be helpful for individuals with IBD who experience these symptoms.
- Specific Carbohydrate Diet (SCD): The SCD is a restrictive diet that eliminates certain carbohydrates believed to contribute to inflammation. Some individuals with IBD have reported improvement in symptoms with this diet.
- Anti-Inflammatory Diet: An anti-inflammatory diet focuses on foods that reduce inflammation in the body. This includes foods rich in omega-3 fatty acids, such as fish and flaxseed, as well as fruits, vegetables, and whole grains.
The Psychological Impact of IBD
Living with IBD can have a significant psychological impact. The chronic nature of the disease, coupled with unpredictable flare-ups and the need for ongoing medical care, can lead to feelings of anxiety, depression, and isolation. It is important to address the psychological aspects of IBD to improve overall well-being and quality of life.
Common Psychological Challenges:
- Anxiety and Depression: The uncertainty of IBD, including the unpredictability of flare-ups and the potential for complications, can lead to anxiety and depression. Individuals may worry about their ability to manage symptoms, maintain employment, and participate in social activities.
- Body Image Issues: Symptoms of IBD, such as weight loss, bloating, and the need for frequent bathroom visits, can impact body image and self-esteem. This can be particularly challenging for adolescents and young adults who may already be dealing with body image concerns.
- Social Isolation: The need to manage symptoms and avoid potential triggers can lead to social isolation. Individuals with IBD may avoid social events, travel, or other activities that could exacerbate their symptoms.
Strategies for Managing Psychological Challenges:
- Counselling and Therapy: Talking to a mental health professional can help individuals with IBD cope with the psychological challenges of the disease. Cognitive-behavioural therapy (CBT) and other therapeutic approaches can provide strategies for managing anxiety, depression, and stress.
- Support Groups: Joining a support group for individuals with IBD can provide a sense of community and connection. Sharing experiences and learning from others who understand the challenges of living with IBD can be empowering and comforting.
- Mindfulness and Stress Reduction: Practices such as mindfulness, meditation, and yoga can help reduce stress and improve mental well-being. These practices can also help individuals develop a greater sense of control over their symptoms and overall health.
The Importance of Regular Medical Care
Regular medical care is essential for managing IBD and preventing complications. This includes routine follow-up appointments with healthcare providers, regular monitoring of disease activity, and adherence to prescribed treatments. Early detection and intervention can help prevent disease progression and improve outcomes.
Key Components of Medical Care for IBD:
- Regular Check-ups: Routine check-ups with a gastroenterologist or primary care provider are important for monitoring disease activity and adjusting treatment as needed. These appointments may include physical exams, blood tests, and imaging studies.
- Medication Management: Medications are a cornerstone of IBD treatment. This may include anti-inflammatory drugs, immune system suppressors, biologics, and other medications. It is important for individuals with IBD to take their medications as prescribed and discuss any side effects or concerns with their healthcare provider.
- Screening for Complications: IBD can lead to complications such as strictures, fistulas, and colorectal cancer. Regular screening and monitoring can help detect these complications early and allow for prompt intervention.
The Future of IBD Research and Treatment
The future of IBD research and treatment is promising, with ongoing advancements aimed at improving the lives of individuals with the disease. Researchers are exploring new therapies, diagnostic tools, and preventive measures to better understand and manage IBD.
Emerging Therapies:
- Biologics and Biosimilars: Biologics are medications that target specific components of the immune system involved in inflammation. New biologics and biosimilars (similar versions of biologic drugs) are being developed to provide more options for patients with IBD.
- Small Molecule Drugs: Small molecule drugs are another area of research, focusing on targeting specific pathways involved in the inflammatory process. These drugs offer the potential for more targeted and effective treatment options.
Personalized Medicine:
- Genetic and Biomarker Research: Advances in genetic and biomarker research are paving the way for personalized medicine in IBD. By identifying genetic markers and biomarkers associated with the disease, researchers can develop more tailored and effective treatment strategies.
Microbiome Research:
- Probiotics and Prebiotics: Research into the role of the gut microbiome in IBD has led to the exploration of probiotics and prebiotics as potential treatments. Probiotics are beneficial bacteria that can help restore a healthy balance in the gut, while prebiotics are substances that promote the growth of these beneficial bacteria.
Inflammatory bowel disease is a complex and challenging condition that affects a significant number of Canadians. From the rising incidence among seniors to the impact on children and the disparities in care for rural populations, IBD presents a multifaceted public health issue. Through ongoing research, improved access to care, and comprehensive support systems, we can work towards a future where the burden of IBD is significantly reduced. By addressing the diverse needs of all Canadians with IBD—whether they are young or old, urban or rural—we can ensure a higher quality of life and better health outcomes for all affected individuals.
-
Hypertension and its Impact on Health
Today, May 17th, is World Hypertension Day, a day dedicated to raising awareness about hypertension and its impact on health. Hypertension, often referred to as high blood pressure, affects as many as 6 million Canadian adults, representing 19% of the adult population. Alarmingly, of those 19%, approximately 17% are unaware of their condition, which underscores the importance of recognizing and managing this health issue. Hypertension is frequently dubbed the “silent killer” because it often presents no symptoms until significant damage has occurred, making it crucial to stay vigilant and informed about this condition.
So what is hypertension, exactly? Blood pressure is the force exerted by blood pumped from the heart against the walls of blood vessels. This force is essential for blood to circulate and deliver vital nutrients and oxygen to organs and tissues throughout the body. High blood pressure occurs when this force is consistently too high, putting undue stress on blood vessels and potentially leading to a variety of health problems. Essentially, anyone can develop high blood pressure, but its prevalence increases with age, making it a common concern as people grow older.
The causes of high blood pressure can be categorized into those that can be managed and those that are beyond one’s control. Lifestyle factors play a significant role in the development of hypertension and include habits such as living a sedentary lifestyle with a lack of regular physical activity, smoking, excessive alcohol consumption, and chronic stress. Additionally, certain medical conditions like diabetes and kidney disease can contribute to high blood pressure. Conversely, factors that are beyond one’s control include age and genetics. Understanding these causes is essential for taking proactive steps to manage and prevent hypertension.
The first step in understanding high blood pressure is learning what your blood pressure numbers mean. Blood pressure is measured with two numbers: systolic and diastolic. Systolic pressure, the higher number, occurs when the heart contracts and pumps blood, while diastolic pressure, the lower number, occurs when the heart relaxes and fills with blood. These measurements are expressed in millimetres of mercury (mmHg), a standardized unit of pressure. For example, a reading of 120/80 mmHg is considered normal. The higher either number is – and the longer it remains elevated – the greater the potential for damage to blood vessels, which can lead to serious health complications.
Uncontrolled high blood pressure poses significant health risks. It increases the likelihood of experiencing a stroke or heart attack, which are both potentially fatal events. High blood pressure can also lead to heart failure, where the heart is unable to pump blood effectively, and increases the risk of developing eye problems that can result in vision loss. Additionally, hypertension is a risk factor for dementia, as it can contribute to the deterioration of cognitive function over time. Kidney disease is another concern, as high blood pressure can damage the blood vessels in the kidneys, impairing their ability to filter waste from the blood. For men, another possible complication of hypertension is erectile dysfunction, which can significantly impact quality of life.
If you have or suspect you might have high blood pressure, it is imperative to speak with your physician. Regular monitoring of your blood pressure is a key aspect of managing the condition. This can be done at home using a blood pressure monitor or by having your healthcare provider check it for you at your doctor’s office or pharmacy. Regular monitoring helps track your blood pressure trends and allows for timely intervention if your numbers start to rise.
World Hypertension Day serves as a reminder of the importance of awareness, prevention, and management of high blood pressure. By understanding the causes, monitoring your blood pressure, and making lifestyle changes where possible, you can take control of your health and reduce the risk of complications associated with hypertension. Staying informed and proactive is the best defense against this silent but deadly condition.
-
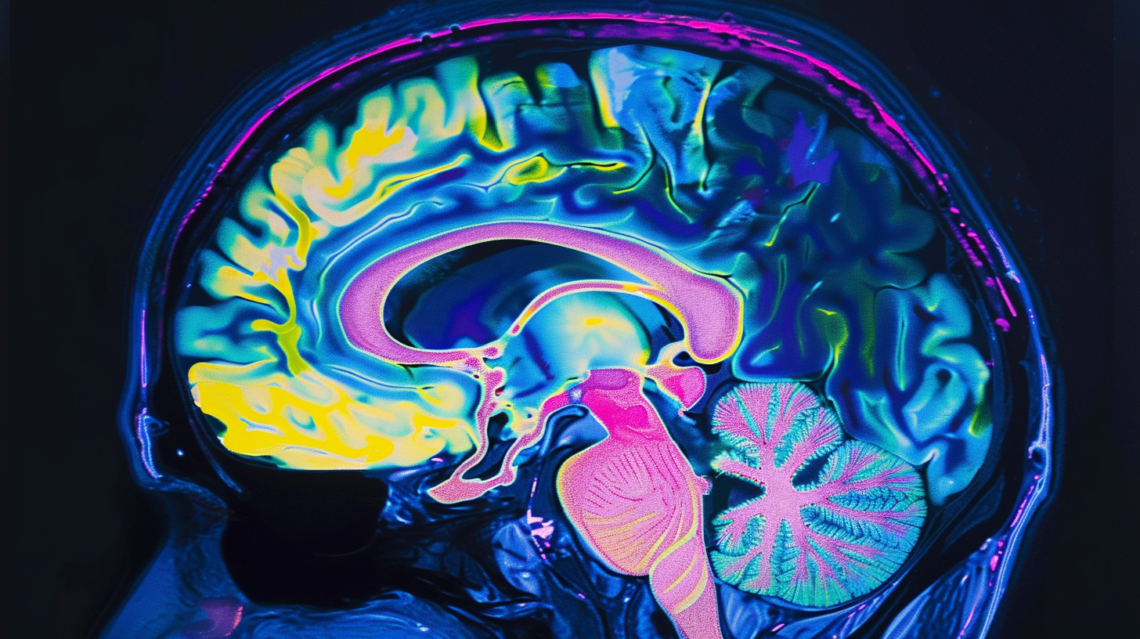
Living with MS in Canada
Canada is recognized as having one of the highest rates of multiple sclerosis (MS) globally, with an estimated 90,000 Canadians currently living with this debilitating disease. The gravity of the situation becomes apparent when considering that, on average, 12 Canadians are diagnosed with MS every single day. This chronic illness predominantly affects individuals between the ages of 20 and 49, marking the beginning of a lifelong struggle against its unpredictable and often progressive nature.
Multiple sclerosis is a complex neurological disorder that targets the central nervous system, encompassing the brain, spinal cord, and optic nerves. Classified as an episodic disability, MS is characterized by its varying severity and duration of symptoms and disability, which can range from mild and transient episodes to more severe and permanent impairments. The disease fundamentally attacks myelin, the protective sheath that envelops nerve fibres, leading to inflammation and, in many cases, significant damage to this critical protective layer. Myelin is essential for the efficient transmission of nerve impulses across the nervous system; hence, even minor damage can cause disruptions in these impulses. In cases where the damage is extensive, scar tissue may form in place of myelin, completely disrupting nerve signal transmission and potentially causing irreversible damage to the nerve fibres themselves.
The unpredictability of MS manifests through a wide array of both physical and mental symptoms. Physically, individuals may experience extreme fatigue, lack of coordination, muscle weakness, tingling sensations, and impaired sensory perceptions. Vision problems, bladder issues, and difficulties with mobility are also common. Mentally, MS can lead to cognitive impairments and significant mood changes, severely impacting a person’s quality of life and their ability to perform daily activities. This variability in symptoms and their progression underscores the complexity of managing and living with the disease.
Diagnosing multiple sclerosis is a meticulous process that relies heavily on a thorough medical history and comprehensive neurological examination. While no single test can definitively diagnose MS, several diagnostic tools are instrumental in confirming the presence of the disease. Magnetic Resonance Imaging (MRI) is often used to detect lesions in the central nervous system, indicative of MS-related damage. Additionally, evoked potential tests, which measure the electrical activity in the brain in response to stimuli, and lumbar punctures, which analyze cerebrospinal fluid, can provide further evidence to support a diagnosis. Critical to the diagnosis of MS is the requirement for evidence of disease activity separated by time (lesions that have formed at different points in time) and space (lesions in at least two distinct areas of the central nervous system). This criterion ensures that the diagnosis reflects the episodic nature of the disease, rather than a singular, isolated incident.
It is crucial to understand that diagnosing MS is a process of exclusion. Physicians must rule out other potential causes for the symptoms before confirming a diagnosis of MS. This comprehensive approach helps ensure that individuals receive an accurate diagnosis, allowing for more effective management and treatment of the disease. The journey to diagnosis can be long and fraught with uncertainty, but it is a vital step towards understanding and managing this complex neurological condition.
In conclusion, the high prevalence of multiple sclerosis in Canada highlights the need for continued research, awareness, and support for those affected by the disease. Understanding the intricacies of MS, from its impact on the nervous system to the diagnostic challenges it presents, is essential for healthcare providers, patients, and their families. As the medical community continues to advance in its knowledge and treatment of MS, there remains a hopeful prospect for better management strategies and, ultimately, a cure for this life-altering disease.
-
Spondyloarthritis
Spondyloarthritis (SpA) is a complex and chronic inflammatory condition that can significantly impact your quality of life. As a physician, it’s essential for me to break down this condition into digestible pieces so that you, as a patient, can understand what you’re dealing with and how to manage it effectively. At its core, SpA refers to a cluster of chronic inflammatory diseases that share common features, both clinically and genetically. These conditions typically manifest with pain and stiffness primarily affecting the back but can also involve other areas of the body, such as the knees, hips, eyes, skin, and gastrointestinal tract.
Central to understanding SpA is recognizing its immune-mediated nature. In simpler terms, your body’s defense system, the immune system, mistakenly attacks its own tissues and cells. Normally, the immune system is adept at identifying and combating foreign invaders like bacteria and viruses. However, in autoimmune diseases like SpA, this system goes haywire, viewing the body’s own cells as threats and launching attacks against them.
The consequence of this autoimmune response is inflammation, which is the hallmark feature of SpA. Inflammation is the body’s natural response to injury or infection, characterized by redness, swelling, heat, and pain. In the case of SpA, this inflammation primarily targets the spine, leading to pain and stiffness. However, what sets SpA apart is that this inflammation isn’t limited to just the spine; it can affect other joints as well. This means that you may experience symptoms in various parts of your body, including your neck, shoulders, hips, or ankles. What’s also crucial to grasp about SpA is that it’s not just a localized issue; it’s a systemic condition. This means that the effects of SpA extend beyond the joints to impact your entire body. You might experience fatigue, fever, and general malaise as your body grapples with the ongoing inflammation and immune dysregulation.
Managing SpA involves a multifaceted approach that aims to reduce inflammation, alleviate symptoms, and improve your overall well-being. This often includes a combination of medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and biologic therapies. Physical therapy and exercise play crucial roles in maintaining joint mobility and function, while lifestyle modifications, such as stress management and healthy eating, can also make a significant difference.
By understanding the underlying mechanisms of the condition and implementing targeted strategies for treatment and self-care, you can take control of your health and minimize the impact of SpA on your daily life.
-
Functional Neurological Disorder
Understanding Functional Neurological Disorder (FND) necessitates a journey into the complexities of how our bodies and brains communicate. This condition, intricate in its nature, affects the nervous system’s functionality, specifically in how the brain and body send and receive signals. In essence, something goes awry in this communication network, leading to a plethora of symptoms that defy easy categorization under known diseases. FND is multifactorial, meaning it can be sparked by a variety of risk factors, both physical and psychological. These contributing elements can intertwine in a manner that makes it challenging to pinpoint a single cause. The resulting symptoms are undeniably real and can significantly impact an individual’s quality of life, sometimes even more so than other neurological conditions that are better understood.
FND’s Unique Position in Medical Science
FND sits at a crossroads of medical disciplines, sharing elements with both neurology and psychiatry, yet not fully residing in either. This unique position underscores the need for a collaborative approach to diagnosis and treatment, one that respects the complexity of the disorder and the person experiencing it. FND is considered a rare condition, but its rarity does not diminish the profound effect it can have on those it touches. A critical aspect of understanding FND is recognizing that the symptoms experienced by patients are not under their conscious control. This is a vital point of clarification, as misconceptions abound regarding the nature of these symptoms.
Symptomatology and Its Impact
Symptoms of FND can appear suddenly and progress rapidly, displaying a tendency to wax and wane over time. This unpredictable pattern can include periods of complete remission, followed by sudden recurrences, adding an element of uncertainty to the lives of those affected. The range of symptoms associated with FND is broad and varied, encompassing chronic pain, cognitive changes (such as difficulties with memory and concentration), alterations in bladder and bowel function, challenges with gait and balance, headaches, involuntary movements, paralysis, weakness, seizures, sensory changes (including altered sensation or hypersensitivity), sleep disturbances, speech problems, and visual changes.
It’s not uncommon for these symptoms to be triggered or exacerbated by another illness or a physical injury. This overlap, often referred to as a ‘functional overlay’, complicates the clinical picture but should not deter the provision of comprehensive care. The presence of FND alongside another medical condition necessitates a nuanced approach to treatment, one that addresses both the symptoms of FND and the concurrent illness without prioritizing one at the expense of the other.
Navigating Treatment and Support
Addressing FND requires a multifaceted strategy, ideally involving a team of healthcare professionals who can offer a range of therapeutic options tailored to the individual’s specific needs. This team might include neurologists, psychiatrists, psychologists, physiotherapists, occupational therapists, and speech therapists, among others. The goal of treatment is not only to manage symptoms but also to improve the overall quality of life for the individual. This can involve physical therapy to address motor symptoms, cognitive-behavioural therapy to help manage the psychological aspects of living with FND, and medication to alleviate specific symptoms such as pain or seizures.
Education plays a crucial role in the management of FND. For patients, understanding the nature of their symptoms and the underlying disorder can be empowering, providing a foundation upon which to build an effective treatment plan. For healthcare providers, knowledge of FND is essential for accurate diagnosis and the development of an empathetic and effective approach to care.
Navigating the complexities of Functional Neurological Disorder calls for a partnership between patients and their healthcare teams, one that is grounded in mutual understanding and respect. The diversity of symptoms and their impact on daily life necessitates a treatment approach that is as unique as the individuals experiencing them. Advances in medical science and a deeper understanding of FND are lighting the path to more effective treatments and improved quality of life. Through collaborative care, embracing both neurology and psychiatry, we are moving toward a future where the challenges of FND can be faced with renewed hope and confidence. In this journey, education and empathy stand as pillars, supporting a framework where patients can navigate their symptoms with dignity and a sense of empowerment.
FND Resources
For comprehensive insights into Functional Neurological Disorder, including frequently asked questions and updates on current research, visit fndhope.org. This resource offers a wealth of information tailored to both individuals navigating the complexities of FND and their supporters, providing a thorough overview of the condition, practical advice, and the latest findings in the field.
-
Managing Spring Asthma
As the first buds of spring begin to appear, many Canadians find themselves looking forward to spending more time outdoors, enjoying the warmer weather. However, for individuals with asthma, the changing seasons can bring about a set of challenges that can affect their ability to enjoy this time of year fully. Spring asthma, as it is commonly referred to, is a condition where asthma symptoms become more pronounced or worsen due to a variety of seasonal triggers. These triggers include pollen from trees, grasses, and flowers, which are abundant in the spring months, as well as changes in temperature and air quality that can accompany the shift from winter to spring. For someone with asthma, exposure to these triggers can lead to inflammation and narrowing of the airways in the lungs, causing symptoms such as wheezing, coughing, shortness of breath, and chest tightness.
Managing spring asthma effectively requires a proactive approach, tailored to the individual’s specific triggers and symptoms. One of the key strategies in managing this condition is the regular use of prescribed asthma medications, which may include inhaled corticosteroids to help reduce inflammation, and bronchodilators to help open up the airways. It’s also crucial for individuals with spring asthma to monitor their symptoms closely and to have a clear action plan in place, developed in consultation with their healthcare provider, to address any potential exacerbations of their asthma promptly. Avoiding known triggers as much as possible is another important aspect of managing asthma. This can include staying indoors on days when pollen counts are particularly high and keeping windows/doors closed to prevent pollen from entering your home. Additionally, wearing a mask when outdoors can also help to reduce the inhalation of pollen and other airborne triggers.
It’s also important to be aware of the impact that asthma can have on an individual’s overall well-being and quality of life. The limitations that asthma symptoms can often impose, especially on things like outdoor activities and exercise, can oftentimes be frustrating, particularly after the long, cold months of winter. However, with careful management and support of healthcare professionals, individuals with spring-exacerbated asthma can still enjoy the beauty and activities of the season. This may involve having to modify outdoor activities to certain times of the day when pollen counts are lower, such as early mornings or later evenings, or finding alternative ways to be active indoors on days when symptoms are more likely to be triggered.
While spring asthma can pose significant challenges, understanding the triggers and symptoms, along with effective management strategies, can help to minimize its impact. By taking these steps to avoid triggers and adhering to medication regimens, you can still look forward to embracing the spring season.
For more spring allergy season tips, visit asthma.ca.
-
Understanding Autism’s Diversity