-
Lung Cancer Signs and Symptoms
Lung cancer is one of the most significant health challenges facing Canadians today, with over 32,000 individuals receiving a diagnosis each year. This staggering number underscores the urgency of understanding, preventing, and treating this complex disease. Lung cancer knows no boundaries, affecting men and women, young and old, smokers and non-smokers alike. It is a stark reminder that, as long as we have lungs, we are all at risk.
While tobacco use remains the leading cause of lung cancer, accounting for the majority of cases, it is not the sole contributor. Environmental factors, such as exposure to radon gas, second-hand smoke, and air pollution, also play a role, as does a family history of the disease. Lung cancer arises when cells in the lung tissue begin to grow uncontrollably, forming tumours that can compromise the vital functions of the lungs. As the disease progresses, it can spread to other parts of the body—a process known as metastasis—making treatment more difficult and reducing the chances of survival.
One of the most troubling aspects of lung cancer is its insidious nature. In its early stages, it often presents no symptoms, allowing the disease to advance unnoticed. By the time signs become apparent, the cancer may have already spread to other parts of the body. Symptoms, when they do occur, can vary widely. Persistent pain in the chest, shoulders, back, or arms may signal the presence of a tumour, while frequent lung infections, such as pneumonia or bronchitis, can be a warning sign. Other symptoms include a chronic cough that does not subside, unexplained fatigue, shortness of breath, and a hoarseness in the voice.
In some cases, the symptoms extend beyond the respiratory system. A loss of appetite or unintentional weight loss can indicate the body is under significant stress. Swelling in the neck or face, dizziness, and weakness are less common but equally concerning signs. In advanced stages, the cancer can lead to bone pain or fractures, blood clots, and even wheezing caused by airway obstruction.
Given the severity of lung cancer and its often late diagnosis, awareness and early detection are crucial. Regular health check-ups and discussions with healthcare providers about risk factors can make a significant difference. Those with a history of smoking or exposure to other risk factors may benefit from low-dose CT scans, which can detect lung cancer in its earliest stages. Quitting smoking, reducing exposure to harmful pollutants, and maintaining a healthy lifestyle are proactive steps everyone can take to lower their risk.
In Canada, lung cancer screening is primarily aimed at individuals deemed to be at higher risk for the disease. Eligibility criteria vary slightly between provinces, but they typically focus on factors such as age and tobacco use history. Additional considerations can include a person’s educational background, ethnicity, family history of lung cancer, personal history of other cancers, body mass index (BMI), and whether they have been diagnosed with chronic obstructive pulmonary disease (COPD). While current screening programs are generally limited to those with a history of smoking, it is essential to emphasise that lung cancer can affect anyone, even those who have never smoked.
For further information about lung cancer, available treatments, and supportive resources, visit LungCancerCanada.ca.
-
National Addictions Awareness Week
National Addictions Awareness Week (NAAW) serves as a pivotal opportunity for Canadians to come together and address the complex and far-reaching impacts of alcohol and other drug-related harms. With its roots in raising awareness and fostering dialogue, this annual event encourages individuals, communities, and organizations across the country to learn more about the critical importance of prevention, harm reduction, treatment, and recovery. By engaging in meaningful conversations and sharing diverse perspectives, NAAW not only shines a spotlight on the challenges associated with substance use but also highlights innovative solutions that can drive positive change at both individual and societal levels.
This year’s theme, Forging Connections, underscores the vital role that human relationships and social networks play in addressing the root causes and consequences of addiction. By fostering stronger connections—whether within families, among friends, in workplaces, or across broader community networks—Canadians can create environments where those struggling with addiction feel supported and empowered to seek help. The theme also emphasizes the need for collaboration among healthcare providers, policymakers, educators, and community leaders to develop and implement evidence-based strategies that prioritize both individual well-being and public health outcomes.
Central to the conversation around NAAW is the recognition that addiction does not occur in isolation. Substance use often intersects with mental health challenges, trauma, socio-economic factors, and systemic inequities. Prevention and harm reduction efforts must therefore take a holistic approach, addressing not only the immediate risks associated with substance use but also the underlying factors that contribute to vulnerability. From public education campaigns that challenge stigma to accessible harm reduction services like supervised consumption sites and naloxone distribution programs, Canada is gradually adopting a more compassionate and pragmatic approach to substance use. Equally important is the focus on treatment and recovery, which are essential components of the broader addiction care continuum. Recovery is not a linear process, and it looks different for everyone. By creating pathways to treatment that are flexible, person-centred, and culturally informed, communities can help individuals navigate their unique journeys towards healing and self-discovery. Support systems, whether through peer groups, counselling services, or residential treatment programs, are invaluable in providing the encouragement and resources needed for sustained recovery.
As Canadians reflect on this year’s NAAW theme, it becomes clear that the path to addressing addiction lies in breaking down barriers and building bridges. Whether it’s through open conversations that challenge stigma, policies that prioritize harm reduction, or community initiatives that bring people together, the act of forging connections has the power to create a society where everyone—regardless of their struggles—feels valued, understood, and supported.
National Addictions Awareness Week is a reminder that while addiction can be deeply isolating, the solutions lie in collective action and shared humanity. By embracing empathy, fostering connection, and advocating for systemic change, Canadians can move closer to a future where addiction is met not with judgment but with care, compassion, and the unwavering belief in the possibility of recovery. Let us seize this moment to not only raise awareness but also to take tangible steps towards building healthier, more inclusive communities that support all individuals in leading fulfilling lives.
-
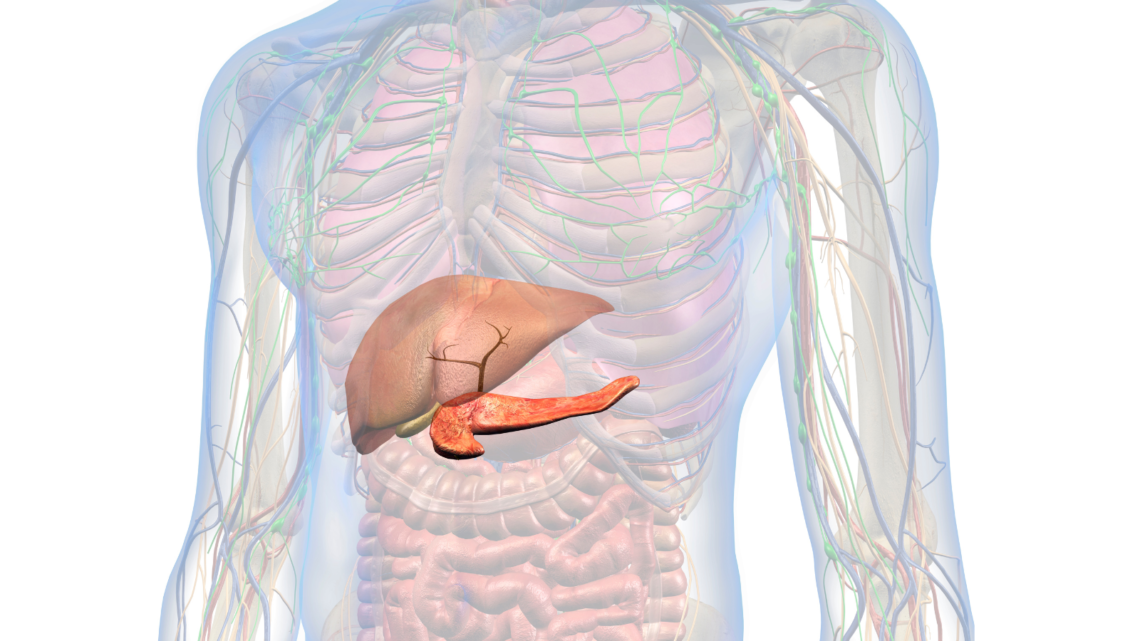
Understanding Pancreatic Cancer Symptoms
Pancreatic cancer, often referred to as a “silent killer,” is one of the most challenging and aggressive forms of cancer that can affect individuals in Canada and around the world. This year alone, it is estimated that approximately 7,100 Canadians will receive the life-altering diagnosis of pancreatic cancer, a figure that underscores the urgent need for greater awareness, earlier detection, and more effective treatment options. The pancreas, a vital organ tucked deep within the abdomen, plays a crucial role in both digestion and blood sugar regulation by producing enzymes that help break down food and hormones like insulin that control glucose levels. Unfortunately, this essential organ’s deep-seated location and its complex functions contribute to the unique challenges of identifying and treating pancreatic cancer at an early stage.
One of the reasons pancreatic cancer is so difficult to detect is that its symptoms often develop insidiously and can easily be mistaken for other, less serious conditions. In the early stages, many individuals experience non-specific symptoms, such as fatigue, abdominal discomfort, back pain, or unexplained weight loss, which may not initially raise alarm. As the disease progresses, more pronounced symptoms may emerge, such as jaundice—a yellowing of the skin and eyes caused by a blockage of the bile duct—dark urine, pale stools, persistent nausea, and loss of appetite. However, by the time these symptoms become noticeable enough to prompt medical investigation, the cancer has often already spread to nearby tissues or other parts of the body, making curative treatment less feasible. This lack of clear early warning signs makes pancreatic cancer notoriously difficult to diagnose promptly, contributing to its poor prognosis and high mortality rate.
Another complicating factor in the detection of pancreatic cancer is the absence of routine screening tests that are both reliable and widely available. Unlike other cancers such as breast or colorectal cancer, which can be detected through mammograms or colonoscopies, there is no standardised screening tool for pancreatic cancer that can be used on a population-wide scale. Imaging studies like CT scans, MRIs, or endoscopic ultrasounds can sometimes identify tumours, but these methods are typically only employed after symptoms arise or if there is a strong suspicion of pancreatic cancer based on family history or genetic predisposition. In many cases, by the time these imaging techniques reveal the presence of a tumour, the disease is already advanced, leaving fewer options for effective treatment. Additionally, the pancreas’s anatomical position—nestled behind the stomach and surrounded by other vital organs—makes it challenging to access and examine, further complicating efforts to detect cancer early.
The subtle onset of pancreatic cancer symptoms and the lack of effective screening tools highlight the importance of understanding individual risk factors and paying attention to one’s health. While the exact causes of pancreatic cancer are not fully understood, certain factors are known to increase the risk of developing the disease, including smoking, obesity, diabetes, chronic pancreatitis, and a family history of pancreatic or related cancers. People with these risk factors should be especially vigilant and seek medical advice if they experience persistent or unexplained symptoms. Unfortunately, even with heightened awareness, the reality remains that pancreatic cancer is often diagnosed at an advanced stage, making it one of the deadliest cancers in Canada and globally.
Despite the bleak statistics, there is hope on the horizon as researchers continue to work tirelessly to better understand pancreatic cancer, develop new treatments, and improve early detection methods. Advances in genomic research and personalised medicine are paving the way for more targeted therapies, while innovative diagnostic techniques, such as liquid biopsies and molecular imaging, hold promise for identifying pancreatic cancer in its earlier stages. Nonetheless, the road to significantly improving outcomes for pancreatic cancer patients remains long, and efforts to raise awareness and support funding for research are critical.
-
Crohn’s and Colitis
Crohn’s disease and colitis, often grouped under the umbrella term ‘inflammatory bowel diseases’ (IBD), represent a significant challenge in the field of gastroenterology. Despite their prevalence and impact, misconceptions and uncertainties about these conditions persist. This article aims to demystify Crohn’s and colitis, delving into their pathophysiology, symptoms, diagnosis, treatment, and the lived experiences of those affected.
At the core, Crohn’s disease and Colitis are chronic conditions characterized by inflammation of the gastrointestinal (GI) tract. However, they exhibit distinct patterns of inflammation and affected areas. Crohn’s disease can affect any part of the GI tract, from mouth to anus, but commonly targets the end of the small intestine and the beginning of the colon. Colitis, specifically ulcerative colitis, is confined to the colon and the rectum. The inflammation in Crohn’s disease tends to be patchy and transmural, affecting the entire thickness of the bowel wall. In contrast, colitis usually involves continuous inflammation of the innermost lining of the colon. These differences in inflammation patterns not only help in distinguishing the two but also influence their symptomatology and complications.
Symptoms and Diagnosis: A Multifaceted Challenge
Both Crohn’s and colitis manifest with a spectrum of symptoms, often overlapping yet distinct in their presentation. Common symptoms include persistent diarrhea, abdominal pain, rectal bleeding, weight loss, and fatigue. Crohn’s disease may also lead to complications such as strictures, fistulas, and abscesses, owing to its transmural inflammation. Colitis, in severe cases, can result in toxic megacolon, a life-threatening complication.
Diagnosing these conditions involves a comprehensive approach. A detailed medical history and physical examination are paramount. Diagnostic tools include blood tests, stool tests, endoscopic procedures like colonoscopy, and imaging studies such as MRI or CT scans. Biopsies taken during endoscopy can be pivotal in confirming the diagnosis and assessing the extent and severity of inflammation.
The Etiological Puzzle: Genetics and Environment
The exact cause of Crohn’s disease and colitis remains elusive, but it is widely acknowledged that a combination of genetic, environmental, and immune factors plays a role. Genetic predisposition is evident, with a higher incidence in individuals with a family history of IBD. Environmental factors, including diet, lifestyle, and exposure to certain microbes, are also believed to contribute to the onset and progression of these diseases.
Treatment Modalities: Tailoring to Individual Needs
Treatment for Crohn’s and colitis is multifaceted and tailored to the severity and location of the disease. The primary goal is to reduce inflammation, manage symptoms, and prevent complications. Medications form the cornerstone of treatment, including aminosalicylates, corticosteroids, immunomodulators, and biologic therapies. These drugs help control inflammation and induce and maintain remission. In cases where medication is ineffective, surgery may be necessary. For Crohn’s disease, this could involve resection of the affected bowel segment, while colitis may require a colectomy in severe cases. It’s crucial to understand that surgery is not a cure but a means to manage complications and improve quality of life.
Living with Crohn’s and Colitis: A Holistic Perspective
Living with Crohn’s or colitis goes beyond managing physical symptoms. These conditions can have profound psychosocial impacts, affecting mental health, personal relationships, and quality of life. Patients often grapple with the unpredictability of flare-ups and the chronic nature of their illness. Comprehensive care, therefore, includes not only medical treatment but also psychological support and lifestyle modifications. Dietary adjustments can help manage symptoms, and stress reduction techniques can be beneficial. Patient education and support groups play a vital role in empowering individuals to cope with their condition.
The Road Ahead: Research and Hope
Research continues to advance our understanding of Crohn’s disease and colitis. Emerging therapies, including newer biologics and stem cell treatments, offer hope for more effective and personalized management. Moreover, ongoing studies into the genetic and environmental aspects of these diseases promise to unravel more of their mysteries.
In conclusion, Crohn’s disease and colitis, as complex and challenging as they are, can be managed effectively with a comprehensive and personalized approach. Understanding these conditions, their impact, and the advancements in their management can empower patients and healthcare professionals alike in navigating these often turbulent waters of inflammatory bowel diseases.
-
Recovering from Exercise-Induced Soreness
Exercise is something we should all engage in in order to stay healthy. By getting regular physical activity, we reap a lot of benefits associated with it. It can help with weight loss, can decrease fatigue, can reduce your risk of developing a chronic disease (such as diabetes and heart disease), can boost brain health, improve your memory and mood, and can even help the skin. It’s also great for your bones and muscles. However, if you’re someone who is more used to living a sedentary lifestyle and not used to exercise, then it’s not uncommon for your muscles to feel sore after a workout. In many cases, it may take a day or two following exercise before you notice the pain begin to set in, which is completely normal. This is referred to as “delayed onset muscle soreness” (DOMS), which can commonly occur as a result of beginning a new exercise routine or changing your exercise routine in any way, as well as increasing the intensity and duration of your workouts. When you make your muscles work harder, this causes microscopic damage to the muscle fibres, which is what results in them feeling sore or stiff.
Post-exercise muscle soreness and stiffness doesn’t just happen to people who aren’t used to exercise, however. It can happen to anyone. Even seasoned athletes. While it may cause one to lose their enthusiasm to want to continue to workout, the good news is that as your body and your muscles adapt to the new physical demands that you’re putting upon them, the soreness is something that should eventually dissipate over time, and you should even find that your stamina increases – meaning your workouts will start to get easier and easier.
As mentioned, DOMS typically does not develop until 1 or 2 days following a workout, ranging from mild to severe, and can occur between 3 and 5 days. Anything beyond that, or pain that is excruciating to the point where you can barely walk or move certain parts of your body, could mean that you have some type of injury, such as a sprain or strain. If this is the case then you’ll want to see your physician as soon as possible so that you not only avoid causing further damage, but so that you can also be referred to a physiotherapist if necessary. Typically, though, muscle pain as a result of workouts should go away on its own without any serious medical intervention being required. There are, however, certain things you can do yourself to try and ease symptoms and relieve pain.
Some things that can help reduce muscle pain include massaging the affected area, as well as alternating between applying hot and cold (such as heating pads and ice packs) to the affected areas. Heat helps to promote blood flow and also helps muscles relax, while cold can reduce inflammation and numb sore tissues. If you’re applying cold to the affected area, it is typically most effective when you apply it within 48 hours of an injury. Always avoid using extreme heat, as this can cause burns, as well as avoid applying ice directly onto the skin. Furthermore, ice should also be avoided if you’re at risk of cramping, as this could make the pain worse. When it comes to choosing between hot and cold, it all depends on the type of injury you’ve sustained, as well as about personal choice. If you’re unsure whether you should use hot or cold, don’t hesitate to ask your physician for their expert opinion. You can also try taking mild pain relievers, such as acetaminophen or ibuprofen.
In order to prevent muscle soreness from exercise, always try to start gradual with any physical activity you do. By starting slow, you give your muscles more time to adapt to the changes which will hopefully minimize the amount of soreness you experience. It can also help to warm up your muscles by stretching both before and after your workout, although there’s no guarantee that this will fully decrease your risk of developing muscle pain or injuries.
-
Osteoporosis Awareness
Osteoporosis is a serious, widespread condition impacting an estimated 2 million Canadians and approximately 44 million Americans. It is a progressive disease in which the quality and density of bone and bone tissue gradually decline, leading to increased fragility of bones and, therefore, a greater risk of fractures and breaks. Over time, osteoporosis can cause debilitating injuries, particularly affecting the shoulders, spine, hips, and wrists, as these areas bear the brunt of the body’s weight and movement. Individuals with osteoporosis often face a significant reduction in quality of life, as the risk of fractures can lead to chronic pain, loss of mobility, and even psychological impacts, such as anxiety over potential falls.
Several risk factors contribute to the development of osteoporosis, and they are varied and wide-ranging. For instance, a diet low in essential nutrients like calcium and vitamin D can lead to weakened bones. Additionally, individuals who engage in excessive dieting, or those who have poor protein intake, may also find themselves at a higher risk of developing this condition. Age is a critical factor; those over the age of 50 are statistically much more likely to develop osteoporosis compared to younger individuals, as bone density naturally decreases with age. Osteoporosis also shows a gender disparity, disproportionately affecting women more than men, though both genders are certainly susceptible. This difference is largely due to hormonal changes, particularly the reduction in estrogen during menopause, which accelerates bone loss in women.
Furthermore, certain health conditions may also elevate the risk of osteoporosis and contribute to an increased likelihood of falls or fractures, which can complicate and compound the condition. For instance, rheumatological diseases, such as rheumatoid arthritis, lead to inflammation and pain in the joints, weakening the musculoskeletal system overall. Conditions linked to vitamin D deficiency, including chronic kidney disease, chronic liver disease, and malabsorption syndromes, also reduce bone strength. Some neurological disorders increase the risk of falls, which is particularly concerning for those with compromised bone density. Each of these conditions can interact with osteoporosis to amplify health risks.
When osteoporosis is suspected, a healthcare provider will typically recommend a specialized bone density scan, commonly referred to as a DXA or DEXA scan, to assess the mineral density within bones. This scan focuses on bones that are most prone to fractures, particularly the lumbar spine, thigh bone, and forearm, while also including other vulnerable areas like the wrists, heels, and fingers. Fortunately, bone density scans involve minimal exposure to radiation, and the test duration is quite short, ranging from about 10 to 30 minutes. The scan results help medical professionals determine the extent of bone density loss, guiding them in making recommendations tailored to the patient’s specific needs.
Taking proactive measures to reduce or delay the onset of osteoporosis is crucial. Ensuring adequate intake of calcium, vitamin D, and protein plays an essential role in maintaining bone health. Ideally, these nutrients should be sourced from natural foods, as they may be better absorbed and utilized by the body. However, if it’s difficult to meet daily nutrient needs through diet alone, vitamin D and calcium supplements offer a widely available and effective alternative. Regular physical activity is equally important, as it strengthens both bones and muscles, enhancing overall stability and reducing the likelihood of falls. Additionally, avoiding smoking and limiting alcohol consumption are key, as both habits not only elevate the risk of osteoporosis but also impair balance, further increasing the risk of falls and injuries.
For individuals interested in learning more about osteoporosis, reliable information and resources can be found on the Osteoporosis Canada website, available at osteoporosis.ca.
-
Health Benefits of Tea
One of the truly wonderful benefits of drinking tea lies in its rich supply of antioxidants, a powerful set of compounds known for their ability to combat free radicals, which are unstable molecules that, if left unchecked, can lead to cellular damage and, in turn, a range of illnesses and diseases. While the human body does indeed produce its own antioxidants, there is certainly no harm in giving your system a little extra boost from external sources. Incorporating foods and beverages rich in antioxidants, like tea, into your diet can not only reduce the likelihood of developing infections but can also serve as a preventative measure against more serious health conditions. This includes a lowered risk of several forms of cancer, such as colorectal, pancreatic, breast, and lung cancer, which are unfortunately all too common in today’s world. By adding tea to your daily routine, you are embracing a simple yet effective means of enhancing your body’s resilience against disease.
Although tea does contain caffeine, it’s worth noting that its caffeine content is significantly lower than what is typically found in a cup of coffee – in fact, it’s up to 50% lower. Caffeine, as many people are aware, is a stimulant that can keep you awake and potentially interfere with your ability to have a restful night’s sleep. Therefore, if you choose tea over coffee, you’re more likely to enjoy better-quality sleep without the stimulating effects of higher caffeine intake. For those who prefer to avoid caffeine altogether and seek a natural way to unwind in the evening, chamomile tea can be a wonderful choice. Not only is chamomile tea naturally free of caffeine, but it’s also deliciously mild and has a pleasant, soothing flavour that can make bedtime a more relaxing experience. Beyond its role as a caffeine-free beverage, chamomile tea is celebrated for its antispasmodic properties, which means it can help relax muscle contractions in the digestive tract, making it particularly beneficial for those who suffer from conditions such as irritable bowel syndrome (IBS). This makes chamomile a dual-purpose tea that both relaxes and aids in digestion.
Moreover, recent research has pointed to a fascinating benefit of tea consumption, particularly when it comes to green tea, which is thought to have protective effects on bone density. Evidence suggests that green tea may play a role in preventing bone loss, a valuable consideration, especially for individuals over the age of 50, when bones naturally begin to weaken, leading to conditions such as osteoporosis and osteoarthritis. These age-related degenerative issues can cause considerable discomfort and reduce mobility, so any habit that may contribute to bone health, such as drinking green tea regularly, could be a worthwhile addition to one’s lifestyle, particularly as part of a broader strategy for maintaining strength and flexibility well into later years.
For individuals who find themselves frequently battling colds or seasonal flu, incorporating tea into your daily routine may provide your immune system with a much-needed boost. Tea has been shown to enhance the body’s immune defenses, making it easier to ward off infections. If you do happen to come down with a sore throat, sipping warm tea can be especially soothing, offering a comforting respite while supporting your immune system’s efforts to recover. So, for those seeking a comforting and beneficial addition to their daily health regimen, tea stands out as a potent, versatile ally.
-
Navigating Grief
Grief is a universal human experience, a complex emotional response to loss that touches every facet of our lives. Whether it is the loss of a loved one, the ending of a cherished relationship, or even the departure of an integral part of our identity, grief can challenge us in ways we never imagined. It forces us to confront the reality of life without what or who we have lost, leaving a profound void that can seem impossible to fill.
This article aims to explore the intricate ways in which grief impacts people. We will examine both its psychological and physiological effects and delve into healthy ways to navigate through it, including the importance of counselling. Grief does not follow a linear path, and there is no one-size-fits-all method for coping, but understanding the processes involved may help individuals find their own path to healing.
The Many Faces of Grief: Understanding Its Complexity
Grief is deeply personal, and its manifestations vary widely from one individual to another. Elizabeth Kubler-Ross’s five stages of grief—denial, anger, bargaining, depression, and acceptance—offer a general framework, but these stages are not experienced in the same order, nor does everyone experience all of them. Grief is often cyclical, and people can revisit stages repeatedly, sometimes feeling different emotions within the same day.
Moreover, the type of loss plays a significant role in how one experiences grief. The death of a loved one is often the most devastating, but losses such as losing a job, a pet, or even the loss of safety following a traumatic event can all elicit profound grief. Society often focuses on bereavement after a death, but it is crucial to validate all forms of grief, as each loss presents unique challenges to those who endure it.
The Impact of Grief on Mental and Physical Health
Grief affects both the body and mind, often in complex and interrelated ways. The emotional response is usually the most apparent, but grief can also manifest in significant physiological symptoms.
Psychological Effects of Grief
Emotionally, grief can feel like an insurmountable burden. People may experience intense sadness, anger, confusion, and even a sense of numbness. Some individuals describe feeling disconnected from reality, as though they are going through life on autopilot. Anxiety can also be a significant aspect of grieving, particularly if the loss was sudden or traumatic. Fear of additional loss, fear for the future, or generalized anxiety about one’s ability to cope may all arise during the grieving process.
Grief can also have a profound impact on one’s cognitive abilities. Difficulty concentrating, forgetfulness, and a sense of mental fog are common symptoms that can disrupt daily activities. Intrusive thoughts—repeated, vivid memories of the loss—can also make it hard for individuals to focus on anything else. Such symptoms are a normal response to loss, yet they can make navigating everyday responsibilities, like work or family obligations, incredibly challenging.
Physical Effects of Grief
Physiologically, grief can take a significant toll on the body. Many people experience fatigue, sleep disturbances, changes in appetite, and a weakened immune system, making them more susceptible to illness. Headaches, stomach pain, and other somatic symptoms are common responses to prolonged emotional distress. In some cases, individuals may even experience symptoms akin to those of a heart attack, a phenomenon often called “broken heart syndrome” or stress-induced cardiomyopathy.
Sleep disruptions are particularly widespread among people who are grieving. Some individuals find it difficult to fall asleep due to overthinking, while others may sleep excessively in an attempt to escape painful emotions. Either extreme can lead to further complications, such as decreased energy levels, a lack of motivation, or increased irritability, ultimately contributing to a cycle that can be challenging to break without intervention.
Grief also often results in a disconnection from one’s own body. Many individuals describe feeling disoriented or numb, which can make it difficult to care for oneself properly. Simple tasks like eating well, exercising, or even keeping up with personal hygiene may fall by the wayside as they focus on managing the overwhelming emotional pain.
Healthy Ways to Grieve: Coping Strategies for Healing
Grieving is not about moving on or forgetting. It is about finding a way to coexist with the pain, integrating it into your life, and eventually rediscovering a sense of normalcy. Below are some healthy ways to grieve that may help individuals navigate their journey.
1. Acknowledge and Express Your Feelings
The first step in healthy grieving is allowing oneself to feel and acknowledge the wide range of emotions that accompany loss. Many people may attempt to avoid their feelings or deny their intensity because they are too overwhelming. However, suppressing emotions can prolong the grieving process and lead to physical symptoms, including increased stress and anxiety.
Expressing grief through different outlets can be incredibly therapeutic. This could be through talking to a trusted friend, writing in a journal, or even creating art or music. By giving oneself permission to mourn and express those feelings, the burden can become lighter over time.
2. Reach Out for Support
Grief can be an isolating experience, especially when people feel that those around them may not understand what they are going through. However, seeking support—whether from friends, family members, or support groups—is an essential part of the healing process. Sharing your experience with someone who listens without judgment can be comforting, and knowing you are not alone can help normalize your emotions.
Support groups are particularly beneficial for individuals who feel that their friends or family may not understand their particular type of loss. Groups for people who have lost loved ones to similar circumstances—such as a death by suicide, miscarriage, or a child’s death—can provide a much-needed sense of community. Connecting with others who have endured similar losses can help people feel understood and validated in a way that is difficult to find elsewhere.
3. Consider Professional Counselling
Counselling is an incredibly effective way to navigate grief, particularly when the symptoms are prolonged or overwhelming. Speaking with a professional allows individuals to explore their emotions in a safe, non-judgmental environment, which can help them process their feelings in a healthier way. Trained therapists can help guide people through the difficult emotions associated with grief, offering practical tools to better manage anxiety, depression, and other challenges that accompany loss.
In Canada, many therapists offer grief counselling as a specialized service, and individuals can often access these services in person or online, which makes them accessible regardless of location. Cognitive behavioural therapy (CBT) is one modality that can be particularly effective for grief, as it can help individuals reframe negative thought patterns and foster a greater sense of hope and resilience.
4. Allow Yourself to Grieve at Your Own Pace
There is no set timeline for grief. Some people may find they are able to resume regular activities relatively quickly, while others need much more time. Both experiences are valid, and comparing one’s journey to that of others can lead to unnecessary feelings of guilt or inadequacy.
Grief does not simply end one day; rather, it tends to soften over time. There may always be moments when the sadness resurfaces, particularly on anniversaries, birthdays, or during significant life events. Recognizing that it is normal to feel a resurgence of grief on such occasions can help people manage these episodes without feeling as though they are regressing.
5. Take Care of Your Physical Health
Self-care is crucial during times of grief, as physical health and emotional well-being are deeply interconnected. Even when motivation is low, simple actions such as staying hydrated, eating balanced meals, and engaging in regular physical activity can help improve mood and alleviate symptoms of grief.
Exercise, in particular, can be very beneficial for those who are grieving. Physical activity releases endorphins, which are natural mood enhancers. Even moderate activities such as walking, yoga, or swimming can help lift one’s mood and provide a much-needed break from the intensity of grief.
6. Create Rituals to Honour the Loss
Finding ways to honour the memory of a lost loved one or a significant loss can help people feel more connected to what they have lost and provide a sense of purpose in their grieving process. This could involve creating a memorial, planting a tree, or holding a special ceremony to remember them. Some individuals find comfort in continuing traditions that the deceased enjoyed, such as cooking their favourite meal on their birthday or visiting a place they loved.
Acts of remembrance can provide a meaningful outlet for grief and allow individuals to feel as though they are still maintaining a connection with their loved one. Over time, these rituals can also evolve into celebrations of life, rather than just reminders of the loss.
7. Give Yourself Permission to Experience Joy
It can be challenging to experience happiness while grieving, as people often feel that they are betraying their loss if they allow themselves to feel joy. Guilt is a common emotion during the grieving process, and many individuals struggle with the idea of moving forward with their lives after a significant loss. However, it is crucial to remember that feeling joy is not a sign of forgetting; rather, it is a sign of healing.
Grief is not about erasing the memory of what was lost but learning to carry it with love while finding new reasons to smile and move forward. Allowing oneself to engage in activities that bring happiness is an important step in reclaiming one’s life, and it is okay to experience joy even amidst sorrow.
Complicated Grief: When Grieving Becomes Chronic
While most individuals gradually adapt to life without what they have lost, some people experience what is known as complicated grief. This condition, also called prolonged grief disorder, occurs when the symptoms of grief are severe, chronic, and impair one’s ability to function in daily life. Complicated grief may include intense yearning for the deceased, difficulty accepting the loss, and a preoccupation with feelings of worthlessness or guilt.
Those experiencing complicated grief may feel stuck in their sorrow, unable to move forward despite the passage of time. They may avoid situations that remind them of the loss or, conversely, become overly preoccupied with these reminders. When grief interferes with one’s ability to engage in everyday activities or leads to prolonged emotional suffering, it is essential to seek professional help.
Treating complicated grief often requires a more intensive therapeutic approach, such as a combination of psychotherapy and medication. Cognitive behavioural therapy and grief-focused therapy are two modalities that have proven effective in helping individuals address complicated grief. Therapists trained in treating complicated grief help individuals process their emotions, confront the reality of their loss, and eventually find ways to rebuild their lives.
Supporting Someone Who Is Grieving
If you know someone who is grieving, you may be wondering how best to support them. The following tips can help you provide meaningful support to someone who is experiencing grief:
1. Be Present
Sometimes, the best support you can offer is simply being there. Grieving individuals may not always want to talk, but having someone by their side can provide immense comfort. Offer to sit with them, hold their hand, or accompany them to appointments. Let them take the lead on whether they want to talk or just need silent companionship.
2. Listen Without Offering Solutions
Many people make the mistake of trying to “fix” the grief of a loved one by offering solutions or advice. In reality, there is no solution for grief, and attempting to provide one can minimize the depth of the loss. Instead, simply listen—without interrupting, judging, or trying to change their emotions.
3. Avoid Clichés and Platitudes
Phrases like “Everything happens for a reason” or “They’re in a better place” are often intended to provide comfort, but they can come across as dismissive or hurtful. Instead of offering clichés, acknowledge the person’s pain by saying something like, “I can’t imagine how hard this is for you, but I’m here if you need anything.”
4. Help with Practical Tasks
Grief can make it difficult to focus on day-to-day responsibilities. Offering to help with practical tasks—such as cooking, cleaning, running errands, or taking care of children—can alleviate some of the burdens that grieving individuals face. Even small gestures can be incredibly impactful during this difficult time.
5. Be Patient
Grief does not have a timeline, and the person you are supporting may need more time than you expect to work through their emotions. They may also experience good days followed by difficult ones. Be patient and let them grieve at their own pace without imposing expectations on when they “should” be feeling better.
Moving Forward: Finding Meaning After Loss
While grief can feel all-consuming, there often comes a point when individuals begin to see glimmers of hope and start to rebuild their lives. This does not mean the grief disappears; instead, they learn to carry it with them in a way that allows them to continue moving forward.
For many, finding meaning in the loss is an essential aspect of healing. This might involve dedicating oneself to a cause that the deceased cared about, creating something in their memory, or using the experience to help others who are grieving. Finding a sense of purpose after loss can help individuals redefine their lives and create something meaningful out of their pain.
Grief is a testament to love. It is an expression of how much someone or something meant to us, and it deserves to be honoured as such. Navigating grief is never easy, and it often leaves people forever changed. However, through healthy coping mechanisms, support, and time, it is possible to carry the memory of what was lost while still finding joy and purpose in the life that remains.
Conclusion: Embracing Grief as Part of the Human Experience
Grief is a complex, deeply personal journey that touches every aspect of our lives. It impacts us emotionally, mentally, and physically, often in profound ways that challenge us to our core. However, by acknowledging our emotions, seeking support, and allowing ourselves to grieve in our own time and manner, we can find ways to heal.
Healthy coping strategies such as reaching out for support, seeking professional counselling, engaging in self-care, and finding ways to honour the loss can all help individuals navigate through grief. It is important to remember that there is no right or wrong way to grieve, and each person’s journey is unique.
Ultimately, grief is an expression of love, a reminder of how deeply we have cared. Embracing it as part of the human experience can help us move forward while keeping the memory of what we have lost alive in our hearts.
If you or someone you know is struggling with grief, consider reaching out for professional help. Support is available, and no one has to endure the pain of loss alone. Whether through therapy, support groups, or simply connecting with others who understand, help is always available, and hope for healing remains within reach.
-
Fall Prevention Month
Fall Prevention Month offers a timely reminder of the importance of safeguarding against falls, a serious and prevalent issue that affects countless individuals, particularly within the aging population. The consequences of falls are not to be underestimated—they are a leading cause of both fatal and non-fatal injuries among older adults, as stated by the Centers for Disease Control and Prevention (CDC). This comprehensive article aims to equip you with a multi-faceted approach to fall prevention, ensuring safety and well-being throughout the autumn of life.
The statistics on falls are sobering. They underscore the urgency of fall prevention, particularly for those advanced in years. The loss of independence, the fear of falling again, and the physical toll of an injury are just a few of the profound impacts a fall can have. It’s not only about the physical pain but also about the psychological and social ripples that follow.
Step 1: Risk Identification
The journey to fall prevention begins with understanding one’s own susceptibility. It is advisable to consult with a healthcare professional who can evaluate risks such as balance deficiencies, chronic conditions that may affect stability, and the potential side effects of medications.
Step 2: Engage in Preventative Exercise
Regular exercise tailored to enhance balance, flexibility, and strength can significantly diminish the risk of falls. Programs should be personalized, and activities like Tai Chi, senior yoga, or even light resistance training can be particularly beneficial.
Step 3: Medication Management
Medications should be routinely reviewed with a healthcare provider to ascertain their role in fall risk. Adjustments or substitutions may be necessary to mitigate side effects like dizziness or impairment that can lead to a fall.
Step 4: Optimize Sensory Health
Since vision and hearing are pivotal in maintaining balance and spatial orientation, regular screenings are critical. Even minor adjustments to prescriptions for glasses or hearing aids can have a significant impact on reducing fall risk.
Step 5: Home Hazard Appraisal
The home environment is a common site for falls, but it can be made safer. This involves:
- Eliminating clutter and securing carpets.
- Ensuring adequate lighting, especially in walkways and night paths.
- Installing support features like grab bars and railing.
- Organizing the household to keep everyday items within easy reach.
Step 6: Appropriate Footwear
The choice of footwear is a simple yet effective fall prevention strategy. Shoes should provide good support, have a non-slip sole, and fit well. Avoiding heels, floppy slippers, and slick soles can prevent unnecessary slips.
Step 7: Nutrition for Bone Health
A diet rich in bone-supporting nutrients like calcium and vitamin D can help prevent the fractures that might result from a fall. A discussion with a nutritionist can help tailor a diet to support bone density and overall health.
Step 8: Community Outreach and Education
Awareness and education are powerful tools in fall prevention. Communities should provide resources and programs to educate the public on fall risks and prevention strategies.
Step 9: Be Prepared for Emergencies
Having a plan in place in the event of a fall is crucial. This includes wearing a personal emergency response system and keeping communication devices within reach, especially for those at high risk.
Step 10: Regular Reevaluation
Fall prevention is not a one-time effort but a continuous commitment. Regular reassessment of one’s living environment and health status is necessary to adapt to changing risks.
Fall Prevention Month is an opportune time to renew commitment to reducing fall risks. Through careful planning, lifestyle adjustments, and community support, we can address the multifaceted challenges of preventing falls. It is through these concerted efforts that we can enhance the safety and quality of life for ourselves and our loved ones, ensuring that the autumn years are enjoyed with stability and peace of mind.
-
Cold Weather & Eczema
Eczema, also known as atopic dermatitis, is a common skin condition marked by itchy, inflamed, and often red patches of skin. As the chilly winter months approach, many Canadians may find themselves struggling with exacerbated symptoms of eczema. Understanding why eczema flares up in winter and adopting appropriate strategies can significantly improve one’s quality of life during these colder months.
Understanding Eczema and Its Winter Woes
Eczema is a chronic condition affecting the skin. It’s characterized by dry, itchy skin and rashes on various parts of the body. The exact cause of eczema remains unknown, but it’s believed to involve a combination of genetic and environmental factors. The condition is often associated with an overactive immune system response to irritants.
Why Winter Hits Hard: During winter, several factors contribute to worsening eczema symptoms:
- Dry Air: Cold air holds less moisture than warm air, leading to drier indoor and outdoor environments. This dryness can strip the skin of its natural moisture, leading to increased irritation and eczema flare-ups.
- Indoor Heating: Central heating systems can further reduce humidity indoors, exacerbating skin dryness.
- Hot Showers and Baths: Seeking comfort in hot baths or showers during cold weather can also strip the skin of its natural oils, worsening eczema.
- Woolen and Synthetic Clothes: Winter clothing often involves materials that can irritate sensitive skin.
Managing Eczema During Winter: Tips and Strategies
1. Humidify Your Environment: Using a humidifier in your home can help maintain an optimal level of humidity, reducing skin dryness.
2. Moisturize Regularly: Applying moisturizer immediately after bathing can help lock in moisture. Choose fragrance-free, hypoallergenic moisturizers that are more gentle on sensitive skin.
3. Gentle Skin Care: Use mild, fragrance-free soaps and avoid scrubbing your skin too hard. Pat dry after washing instead of rubbing.
4. Dress Smartly: Opt for soft, breathable fabrics like cotton instead of irritating materials like wool. Layer clothing to avoid overheating, as sweat can also irritate eczema.
5. Manage Temperature and Humidity: Keep indoor temperatures moderate and consistent. Avoid sudden changes in temperature, which can trigger eczema flare-ups.
6. Stay Hydrated: Drinking plenty of water helps maintain skin hydration from the inside out.
7. Consider a Diet Check: Some foods may exacerbate eczema in certain individuals. It’s worth discussing with a healthcare provider if a diet change could help.
8. Stress Management: Stress is a known trigger for eczema. Techniques like yoga, meditation, or regular exercise can help manage stress levels.
Medical Management
Topical Treatments: These include corticosteroid creams and ointments, which can reduce inflammation and itching. It’s important to use them as directed by a healthcare professional.
Systemic Medications: For severe cases, oral medications or biologics might be prescribed to control the immune system’s overreaction.
Phototherapy: Exposing the skin to controlled amounts of natural sunlight or artificial UV light can improve symptoms for some people.
Skin Barrier Creams: These are designed to repair the skin barrier and are often used in conjunction with other treatments.
When to See a Doctor
Consult a healthcare provider if:
- Eczema symptoms significantly worsen or don’t respond to over-the-counter treatments.
- The skin becomes painful, red, or swollen, which could indicate an infection.
- Eczema interferes with daily activities or sleep.
While eczema can be more challenging to manage in winter, understanding the triggers and adopting a comprehensive skin care routine can make a significant difference. Regular consultation with healthcare providers, personalized skincare strategies, and lifestyle adjustments can help individuals with eczema navigate the winter months with greater ease and comfort.
By staying informed and proactive, those affected by eczema can not only manage their symptoms effectively but also enjoy the winter season with minimal discomfort.