-
Acne: Types, Treatments and Impact on Self-Esteem
Acne is a skin condition that affects a significant portion of the Canadian population, with estimates suggesting that as many as 5.6 million individuals grapple with this issue at some point in their lives. While the condition is most commonly associated with adolescence, affecting an astounding 80 to 90 percent of teenagers, it’s important to note that acne doesn’t discriminate based on age, as it also impacts 20 to 30 percent of adults between the ages of 20 and 40. Although acne is often colloquially referred to as “pimples,” the reality of this skin condition is far more complex and multifaceted than this simplistic term might suggest. In fact, dermatologists recognize three distinct subtypes of acne, each with its own unique characteristics and treatment approaches, as well as six different manifestations that can appear on the skin.
Acne Subtypes and Manifestations
The three primary subtypes of acne are comedonal acne, inflammatory acne, and cystic acne. Each of these subtypes can manifest in various ways on the skin, leading to the six recognized types of acne lesions: whiteheads, blackheads, papules, pustules, nodules, and cysts. Understanding these different forms is crucial for both patients and healthcare providers in developing effective treatment strategies.
Comedonal Acne
Comedonal acne is one of the most frequently diagnosed forms of acne, characterized by the formation of comedones when excess oil and debris become trapped beneath the hair follicles. This subtype encompasses both whiteheads and blackheads, which are often the first visible signs of acne development.
Whiteheads, also known as closed comedones, appear on the skin as white or skin-coloured bumps that can vary in size from small to medium. These lesions occur when the pore is completely blocked, preventing the sebum and dead skin cells from reaching the surface. The white appearance is due to the lack of exposure to air, which prevents oxidation of the trapped material.
Blackheads, or open comedones, share a similar formation process to whiteheads but differ in their appearance due to their open nature. Contrary to popular belief, the dark colouration of blackheads is not caused by dirt, but rather by the oxidation of melanin when exposed to air. This oxidation process gives blackheads their characteristic black or dark appearance, which can sometimes be mistaken for dirt by those unfamiliar with the condition.
Inflammatory Acne
Inflammatory acne represents a more advanced stage of the condition, where the body’s immune response becomes involved, leading to redness, swelling, and potential pain. This subtype includes papules and pustules.
Papules develop when excess dead skin cells and oil clog the pores, potentially accumulating pus and forming small, skin-coloured bumps known as comedones. These comedones can rupture, leading to inflammation and the formation of red, tender bumps on the skin. Papules mark the transition from non-inflammatory to inflammatory acne and can be a precursor to more severe forms if left untreated.
Pustules are often what people envision when they think of classic acne. These lesions appear as red bumps with a white or yellow centre, filled with pus. Pustules typically develop when papules become infected with bacteria, triggering a more pronounced inflammatory response from the body. While it may be tempting to pop these lesions, doing so can lead to further inflammation, scarring, and spread of bacteria.
Cystic Acne
Cystic acne is considered the most severe form of acne and encompasses both nodules and cysts. This type of acne often requires more aggressive treatment and can have a significant impact on an individual’s quality of life due to its painful nature and potential for scarring.
Nodules are a more severe manifestation of acne that form deeper within the skin than other types of acne lesions. They appear as small bumps that can be either skin-coloured or red and are characterized by their firm, hard texture. Nodules are often painful to the touch and can persist for weeks or even months if left untreated. Their deep-seated nature makes them particularly resistant to over-the-counter treatments, often requiring prescription medications for effective management.
Cysts represent the most severe form of acne lesions. Unlike the aforementioned types, which typically appear as smaller bumps on the skin or face, cysts are much larger and more prominent. These lesions form deep within the skin and are filled with pus, dead skin cells, and bacteria. Cysts can be extremely painful and are the most likely form of acne to result in permanent scarring. Due to their severity, cysts often require professional medical intervention, including oral medications or even surgical procedures in some cases.
Acne Management: Do’s and Don’ts
One of the most common and potentially harmful habits that individuals with acne develop is the urge to pop or squeeze their pimples. While it may seem like a quick fix to eliminate a visible blemish, this action can have serious consequences and should be avoided at all costs. When you pop a pimple, you risk spreading pus and infected bacteria to surrounding pores, potentially exacerbating the problem and creating new breakouts. Moreover, this seemingly innocuous action can lead to delayed healing time and, in more severe cases, result in permanent acne scarring that can be difficult or impossible to reverse.
To effectively prevent acne breakouts, it’s crucial to maintain a consistent and gentle skincare routine. This includes washing your face twice daily using a mild, non-comedogenic cleanser that won’t clog your pores. It’s important to note that harsh cleansers and soaps should be avoided, as they can strip the skin of its natural oils, potentially triggering more breakouts as your skin overcompensates by producing excess sebum. Additionally, factors such as stress, diet, and hormonal changes have been known to trigger acne in some individuals. To better understand your personal acne triggers, consider keeping a detailed journal where you can record potential correlations between your lifestyle factors and acne flare-ups. This information can be invaluable when discussing treatment options with your healthcare provider.
The Psychological Impact of Acne
The effects of acne extend far beyond the physical manifestations on the skin. Regardless of the type or severity of acne an individual experiences, this skin condition can have a profound impact on one’s body image and self-esteem. Many people with acne report feeling embarrassed, unattractive, and lacking in confidence, which can lead to a cascade of negative psychological consequences. In some cases, individuals may begin to socially isolate themselves out of fear of how they might be perceived by others, potentially leading to the development of social phobia. This type of social withdrawal can be particularly detrimental, as it may result in individuals becoming house-bound and can even contribute to the onset or exacerbation of anxiety and depression.
If you find that your acne is significantly affecting your ability to socialize with others or carry out your normal daily routines, it’s crucial to be open and honest with your physician about these feelings. Mental health is an integral part of overall well-being, and addressing these concerns should be a key component of your acne treatment plan.
The path to improvement often begins with a referral to a dermatologist, a medical specialist trained in diagnosing and treating skin conditions. A dermatologist can work with you to develop a personalized treatment plan tailored to your specific type of acne and skin needs. As you begin to see improvements in your skin condition, you may notice a corresponding boost in your self-esteem and overall mental well-being.
For additional support, many individuals find it beneficial to join online support groups or forums dedicated to acne and skin health. These communities can provide a sense of solidarity and shared experience that can be incredibly comforting. However, it’s important to approach any medical advice shared in these groups with caution. Always verify information with your physician or dermatologist before making changes to your treatment regimen, as what works for one person may not be suitable or safe for another.
While acne can be a challenging and complex condition to navigate, understanding its various forms, implementing proper skincare practices, and addressing both the physical and psychological aspects of the condition can lead to significant improvements in both skin health and overall quality of life. Remember, you’re not alone in this journey, and with the right support and treatment, clearer skin and renewed confidence are achievable goals.
-
Staying Healthy As You Age
Aging is an inevitable part of life, a journey we all embark upon from the moment we’re born. While we cannot halt the march of time, we do have considerable influence over how we experience the aging process. Numerous factors contribute to how we age, including underlying health conditions, genetic predispositions, and the environment in which we live. However, the choices we make in our daily lives – from the foods we consume to the activities we engage in – play a pivotal role in determining our health and well-being as we grow older. Our lifestyle choices and mental health are particularly significant in the aging process. The habits we form, both good and bad, can have long-lasting effects on our bodies and minds. For instance, chronic stress can accelerate cellular aging, while regular exercise can help maintain cognitive function and physical vitality. It’s never too late to make positive changes that can impact how we age, and understanding this empowers us to take control of our health destiny.
Recent studies have shown that people are living longer now than at any other time in history. A United Nations report highlights this trend, with life expectancy continuing to rise globally. In Canada, for example, women can expect to live to an average age of 81, while men have an average life expectancy of 79 years. This increase in longevity is a testament to advancements in healthcare, improved living conditions, and greater awareness of health-promoting behaviors. However, living longer doesn’t necessarily equate to living better. As we age, our bodies undergo numerous changes, both visible and invisible. Our skin loses elasticity, our bones may become more brittle, and our organs might not function as efficiently as they once did. Cognitive changes can also occur, with some individuals experiencing a decline in memory or processing speed. Yet, many of these changes can be mitigated or slowed through proactive health measures.
So, how can we stay as healthy as possible while aging? Let’s delve deeper into some key areas that can make a significant difference in our health as we grow older.
Foods
The foods we eat play a crucial role in our overall health and can significantly impact the aging process. A diet rich in nutrient-dense foods can help combat the effects of aging from the inside out. Fruits and vegetables, in particular, are powerhouses of anti-aging compounds. Foods like broccoli, spinach, and kale are rich in antioxidants that fight free radicals, which are known to accelerate aging at a cellular level. Avocados provide healthy fats that support skin health and cognitive function. Sweet potatoes offer beta-carotene, which the body converts to vitamin A, supporting eye health and immune function.
Berries, especially blueberries, are often touted as superfoods due to their high antioxidant content. They’ve been linked to improved memory and cognitive function in older adults. Pomegranates and papayas are rich in vitamins and compounds that support skin health, potentially reducing the appearance of fine lines and wrinkles. Nuts, such as almonds and walnuts, provide healthy fats, protein, and vitamin E, which can support heart and brain health.
Incorporating these foods into your diet isn’t just about looking younger; it’s about feeling younger too. These nutrient-rich foods can help reduce inflammation in the body, a process that’s linked to many age-related diseases. They can strengthen cell membranes, making our bodies more resilient to stress and environmental damage. Moreover, a diet rich in fruits, vegetables, whole grains, and lean proteins can promote heart health, support brain function, and even reduce the risk of certain cancers and respiratory diseases.
It’s important to note that while these foods have powerful health benefits, they’re not magic bullets. The key to reaping their benefits lies in consistency and variety. Aim to include a wide range of colorful fruits and vegetables in your diet, along with whole grains, lean proteins, and healthy fats. Remember, it’s never too late to improve your diet. Even small changes, like adding an extra serving of vegetables to your meals or swapping out processed snacks for fruit, can make a significant difference over time.
Exercise
Physical activity is another crucial component of healthy aging. Regardless of your current age or fitness level, increasing your physical activity can yield significant health benefits. Regular exercise isn’t just about maintaining a healthy weight; it’s about keeping your body functioning optimally as you age.
One of the most accessible and beneficial forms of exercise, especially for older adults, is walking. It’s low-impact, requires no special equipment, and can be done almost anywhere. Regular walking can improve cardiovascular health, strengthen bones, enhance balance and coordination, and even boost mood and cognitive function. Studies have shown that older adults who walk regularly have a lower risk of dementia and better overall cognitive function.
For those who enjoy water-based activities or have joint issues that make land-based exercises challenging, water aerobics can be an excellent option. The buoyancy of water reduces stress on joints while providing resistance for strength training. Water aerobics can improve flexibility, strength, and cardiovascular fitness, all while being gentle on the body.
Gardening is another activity that combines physical exercise with the joy of nurturing plants. It provides a full-body workout, improving strength, flexibility, and endurance. Moreover, spending time in nature and caring for plants can have significant mental health benefits, reducing stress and promoting a sense of accomplishment and connection to the natural world.
The key to reaping the benefits of physical activity is consistency. Find activities you enjoy and make them a regular part of your routine. Even small amounts of activity, spread throughout the day, can add up to significant health benefits. Remember to start slowly and gradually increase your activity level, especially if you’ve been sedentary. Always consult with your healthcare provider before starting a new exercise regimen, particularly if you have any existing health conditions.
Sleep
Sleep is often overlooked in discussions about healthy aging, but it’s a critical component of overall health and well-being. As we age, our sleep patterns naturally change. Many older adults find they have trouble falling asleep, wake up more frequently during the night, or wake up earlier in the morning. While some changes in sleep patterns are normal, chronic sleep deprivation can have serious health consequences.
Adequate sleep is essential for physical restoration, cognitive function, and emotional well-being. During sleep, our bodies repair tissues, consolidate memories, and regulate hormones. Chronic sleep deprivation has been linked to an increased risk of obesity, diabetes, cardiovascular disease, and even certain types of cancer. It can also affect cognitive function, leading to problems with memory, concentration, and decision-making.
To improve sleep quality, it’s important to establish good sleep hygiene habits. This includes maintaining a consistent sleep schedule, even on weekends. Our bodies thrive on routine, and a regular sleep-wake cycle can help regulate our internal clock. Creating a relaxing bedtime routine can also signal to your body that it’s time to wind down. This might include activities like reading a book, listening to calming music, or practicing gentle stretching or meditation.
The sleep environment is also crucial. Ensure your bedroom is dark, quiet, and cool. Invest in a comfortable mattress and pillows. Avoid screens (TV, smartphones, tablets) for at least an hour before bed, as the blue light emitted by these devices can interfere with the production of melatonin, a hormone that regulates sleep.
Be mindful of what you consume in the hours leading up to bedtime. Avoid caffeine in the afternoon and evening, as its stimulant effects can last for several hours. While alcohol might help you fall asleep initially, it can disrupt sleep later in the night, leading to poor sleep quality. Similarly, heavy meals close to bedtime can cause discomfort and interfere with sleep.
If you find you’re having persistent trouble sleeping, it’s important to consult with your healthcare provider. Conditions like sleep apnea, restless leg syndrome, or chronic pain can significantly impact sleep quality and may require medical intervention. Your doctor may recommend cognitive behavioral therapy for insomnia (CBT-I), a type of therapy specifically designed to improve sleep, or in some cases, may suggest short-term use of sleep medications.
Remember, good sleep is not a luxury; it’s a necessity for healthy aging. Prioritizing sleep is one of the most important things you can do for your overall health and well-being as you age.
Other Lifestyle Factors
In addition to diet, exercise, and sleep, there are many other lifestyle factors that can contribute to healthy aging. Staying socially active, for instance, is crucial for mental health and cognitive function. Engaging in community activities, maintaining close relationships with friends and family, or volunteering can provide a sense of purpose and connection that’s vital for emotional well-being.
Challenging your mind is equally important. Learning new skills, taking up a hobby, or engaging in puzzles and brain games can help maintain cognitive function and potentially reduce the risk of age-related cognitive decline. The concept of neuroplasticity suggests that our brains continue to form new neural connections throughout life, especially when we engage in novel and challenging activities.
Stress management is another key component of healthy aging. Chronic stress can accelerate the aging process, affecting everything from our immune system to our cardiovascular health. Techniques like meditation, deep breathing exercises, or yoga can help manage stress levels and promote overall well-being.
Regular health check-ups are crucial as we age. Many health conditions are more easily treated when caught early, so staying on top of recommended screenings and check-ups is important. This includes not just physical health, but also dental and eye health, which can have significant impacts on overall quality of life.
Staying hydrated is a simple but often overlooked aspect of health. As we age, our sense of thirst may diminish, making it easier to become dehydrated. Adequate hydration is crucial for numerous bodily functions, from maintaining skin health to supporting kidney function.
Bad Habits
Lastly, it’s important to address harmful habits. Smoking and excessive alcohol consumption can accelerate the aging process and increase the risk of numerous health problems. It’s never too late to quit smoking or reduce alcohol intake, and doing so can have immediate and long-term health benefits.
While aging is an inevitable part of life, how we age is largely within our control. By making informed choices about our diet, staying physically active, ensuring we get quality sleep, and adopting other healthy lifestyle habits, we can significantly enhance our quality of life as we grow older. Aging doesn’t have to mean decline; with the right approach, it can be a time of continued growth, learning, and vitality. Remember, small changes made consistently over time can lead to significant improvements in health and well-being. Embrace the journey of aging with positivity and proactivity, and you’ll be well on your way to a healthier, happier later life.
-
Staying Healthy This Fall
As summer fades and autumn approaches, the changing seasons bring new health challenges. With shorter days, shifting weather patterns, and the looming cold and flu season, it’s crucial to prioritize your well-being. Below are some valuable tips to help you maintain good health throughout the fall months.
Warding Off Seasonal Illnesses
While the official cold and flu season in Canada typically begins in November, there’s often a noticeable uptick in viral and bacterial infections from September to October, coinciding with the back-to-school period. To minimize your risk of falling ill:
- Practice rigorous hygiene: Wash hands frequently with warm water and soap, and keep hand sanitizer readily available when soap and water aren’t accessible.
- Avoid spreading germs: Stay home when you’re sick, and steer clear of those who are ill.
- Use proper etiquette: Cough or sneeze into a tissue or your sleeve rather than your hands.
- Follow medical advice: If prescribed antibiotics for bacterial infections like pneumonia or sinusitis, complete the entire course as directed. Failing to do so may lead to recurring or worsening infections and contribute to antibiotic resistance.
Embracing Autumn’s Bounty
The Pumpkin Craze
While “pumpkin spice season” brings an array of tempting treats, many are laden with sugar and unhealthy additives. However, pumpkin itself offers numerous health benefits:
- High in fibre
- Rich in potassium and beta-carotene
- Pumpkin seeds are excellent sources of magnesium and protein
Consider incorporating pure pumpkin into your diet through homemade soups, roasted vegetable medleys, or as a nutrient-dense addition to smoothies.
Apples: Nature’s Health Food
The old adage “an apple a day keeps the doctor away” holds more truth than you might think. Apples are particularly abundant in autumn and offer several health benefits:
- High in antioxidants and vitamin C
- Rich in soluble fiber, which can help lower cholesterol
- Associated with reduced risk of heart disease and stroke
Try incorporating apples into your diet through fresh snacks, baked desserts (in moderation), or as a crunchy addition to salads.
Staying Active Outdoors
After a scorching summer, fall’s milder temperatures provide ideal conditions for outdoor exercise. Benefits of outdoor physical activity include:
- Boosted energy levels
- Stress relief
- Improved mood and mental health
Take advantage of sunny autumn days by:
- Going for walks or jogs in local parks
- Hiking scenic trails
- Cycling through colorful foliage
- Participating in outdoor yoga or fitness classes
Additional Fall Health Tips
- Stay hydrated: Although the weather is cooler, it’s still important to drink plenty of water.
- Get enough sleep: As days shorten, adjust your sleep schedule to ensure you’re getting 7-9 hours of quality rest.
- Boost your immune system: Consider taking vitamin D supplements, as reduced sunlight can lead to deficiencies.
- Prepare for allergies: Fall allergies can be just as severe as spring ones. Consult with your doctor about managing seasonal allergies.
- Mind your mental health: The transition to fall can impact mood. Stay connected with loved ones and consider light therapy if you’re prone to seasonal affective disorder.
By following these tips and embracing the unique opportunities that autumn offers, you can maintain and even improve your health as the seasons change. Remember, prevention is always better than cure, so take proactive steps to safeguard your well-being this fall.
-
Ovarian Cancer: What You Need to Know
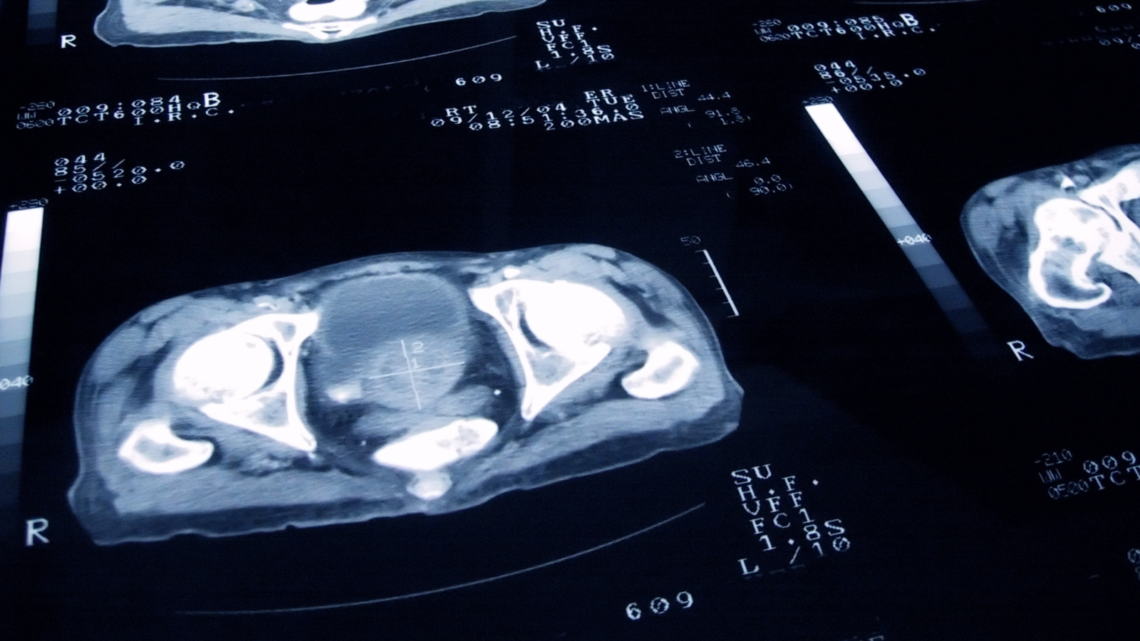
Ovarian cancer is a group of distinct malignancies that originate in or near the ovaries, which are the female reproductive glands located in the lower abdomen on either side of the uterus. These essential organs are responsible for producing eggs (ova) for reproduction, as well as the crucial female hormones oestrogen and progesterone. The ovaries are composed of three primary cell types: epithelial cells, which form the outer surface of the ovary; germ cells, found within the ovary and responsible for egg production; and stromal cells, which comprise the structural tissue that maintains the ovary’s integrity. Each of these cell types has the potential to develop into a different type of tumour, leading to the broad classification of ovarian cancers based on their cellular origin. It is important to note that while ovarian tumours can be benign (non-cancerous), malignant (cancerous) ovarian tumours have the ability to spread (metastasize) to other parts of the body, potentially resulting in serious health consequences.
Symptoms of Ovarian Cancer
While every individual born with ovaries carries some risk of developing ovarian cancer, certain factors can significantly increase one’s susceptibility to this disease. Age, ethnicity, and genetics play crucial roles in determining an individual’s risk profile, and it is worth noting that those who have previously been diagnosed with breast cancer face an elevated risk of ovarian cancer as well. Recognizing the symptoms of ovarian cancer is vital for early detection and improved treatment outcomes, although this can be challenging due to the often vague and nonspecific nature of the symptoms. Common indicators may include persistent bloating, abdominal or pelvic pain and discomfort, difficulty eating or feeling full quickly, and changes in urinary habits. Less frequent symptoms can encompass alterations in bowel habits, nausea, fatigue, unexplained weight loss, postmenopausal bleeding, menstrual irregularities, back pain, indigestion, pain during intercourse, and bleeding after sexual activity.
Diagnosing Ovarian Cancer
The diagnosis of ovarian cancer presents numerous challenges, primarily due to the absence of a reliable screening test and the lack of a single, definitive diagnostic tool. The symptoms associated with ovarian cancer often mimic those of more common and benign conditions, further complicating the diagnostic process. Moreover, the most prevalent form of ovarian cancer tends to spread when the cancer cells are still microscopic, often before any noticeable symptoms manifest. Consequently, ovarian cancer is frequently diagnosed in its later stages (Stages 3 and 4), which can have a detrimental impact on survival rates. It is crucial to dispel the common misconception among Canadians that the HPV vaccine and Pap test, which are associated with cervical cancer prevention and detection, are effective against ovarian cancer. While significant global research efforts are underway to develop a reliable screening test for early-stage ovarian cancer detection, no such test currently exists with sufficient sensitivity. Therefore, it is imperative for individuals experiencing persistent symptoms lasting three weeks or more to consult their physician promptly. Diagnostic procedures that may aid in the detection of ovarian cancer include pelvic examinations and transvaginal ultrasounds.
Treating Ovarian Cancer
The treatment approach for ovarian cancer is highly individualized, taking into account factors such as the stage and grade of the cancer, the type and size of the tumour, the patient’s age and overall health, and whether it is a new or recurring diagnosis. Surgery often serves as the initial step in treating most ovarian cancers and plays a crucial role in staging the disease. During the surgical procedure, the tumour is removed and subsequently examined by a pathologist to determine the stage and grade of the ovarian cancer, which informs the gynecologic oncologist’s treatment decisions. Chemotherapy is frequently employed in ovarian cancer treatment, either before or after surgery, typically involving a combination of two different drugs. The primary drug is usually a platinum-based compound, such as cisplatin or carboplatin, while the secondary drug is often a taxane, such as Taxol or Taxotere. Additional chemotherapy agents may be utilized to extend survival. Radiation therapy, which employs high-dose radiation to destroy cancer cells and damage their DNA, preventing further division and growth, can also be an effective treatment option for ovarian cancer. This approach may be particularly beneficial in cases where minimal residual cancer remains after debulking surgery or in instances of ovarian cancer recurrence.
For those seeking additional information and support regarding ovarian cancer, OvarianCanada.org serves as a valuable resource, offering comprehensive guidance and up-to-date research.
-
Preventing Concussions
With thousands of children and teenagers now back to school and also partaking in after-school activities, it’s not uncommon to see contact sport-related injuries on the rise such as sprains, bone fractures and concussions. A concussion occurs when the brain impacts the inside of the skull, usually the result of direct trauma to the head, and causes damage that ultimately changes how your brain cells function.
While concussions are common among athletes and school-aged children, kids and adolescents are also at higher risk of developing a concussion due to the fact that their brains are still growing. Symptoms of conclusions can be physiological (including headaches, dizziness and nausea, cognitive (including lack of concentration, memory loss and slurred speech), as well as emotional (depression and anxiety.) As concussions can have serious and sometimes life-altering effects, it is important that these symptoms are taken seriously and treated immediately. It is also important to watch out for late signs of a concussion, as symptoms can take as long as hours, days, or even weeks to develop. If left untreated, a concussion can lead to a traumatic brain injury (500 out of every 100,000 Canadians are diagnosed with a TBI each year), and can even be fatal.
Children are not the only age group at high-risk of developing concussions, however. Seniors are also susceptible to developing concussions, usually the result of a fall, something that is quite common with age. Studies have also shown that seniors with concussions had a greater risk of developing Alzheimer’s disease as opposed to those who have not had any previous head injuries. Seniors that do develop a concussion may require hospitalization and long-term rehabilitative care depending on the severity of the injury.
In order to prevent a concussion, one should always ensure that they are taking appropriate steps to reduce that risk. These steps include wearing the proper headgear and padding during sports, wearing appropriate footwear, wearing a seatbelt while in a vehicle, and keeping your home safe by moving any clutter and keeping dark spaces well lit. Regular, low-impact exercise in older individuals will also help to strengthen the bones and muscles, improve balance, and decrease the risk of falls.
-
Prostate Cancer in Canadian Men
Prostate cancer stands as one of the most prevalent and concerning health issues affecting Canadian men today. As a disease that predominantly affects older males, it has far-reaching implications not only for individuals but also for families, communities, and the healthcare system at large. This comprehensive article aims to shed light on the various aspects of prostate cancer, from its incidence and risk factors to its symptoms and impact on Canadian society. By delving into the intricacies of this condition, we hope to provide valuable insights that can empower men and their loved ones with the knowledge needed to navigate this challenging health landscape.
The Scope of Prostate Cancer in Canada
The magnitude of prostate cancer’s impact on Canadian men cannot be overstated. Recent statistical projections paint a sobering picture of the disease’s prevalence in the country. It is estimated that in 2024, a staggering 27,900 Canadian men will receive a diagnosis of prostate cancer. This figure is not just a number; it represents a significant portion of the male population whose lives will be profoundly affected by this disease. To put this into perspective, prostate cancer is expected to account for 22% of all new cancer cases in men in 2024. This means that more than one in five new cancer diagnoses among Canadian men will be prostate cancer, underscoring its position as a major public health concern.
The implications of these statistics are far-reaching. They indicate that a substantial number of Canadian families will be touched by prostate cancer in some way, whether directly through a diagnosis or indirectly through the diagnosis of a loved one. This prevalence also places a significant burden on the healthcare system, necessitating substantial resources for screening, diagnosis, treatment, and ongoing care. Moreover, these numbers highlight the critical importance of awareness, early detection, and research into more effective treatments and potential preventive measures.
It’s important to note that while these statistics are alarming, they also reflect advancements in screening and diagnostic techniques. Improved methods of detection mean that more cases of prostate cancer are being identified at earlier stages, potentially leading to better outcomes for many patients. However, this high incidence rate also underscores the need for continued vigilance and proactive health measures among Canadian men, particularly as they age.
Understanding Prostate Cancer
Before delving deeper into the specifics of prostate cancer in the Canadian context, it’s crucial to establish a foundational understanding of what prostate cancer is and how it develops.
The prostate is a small, walnut-sized gland located just below the bladder and in front of the rectum in men. It plays a vital role in the male reproductive system, producing seminal fluid that nourishes and transports sperm. Prostate cancer occurs when cells in the prostate gland begin to grow and divide uncontrollably, forming a tumour that can potentially spread to other parts of the body if left untreated.
Like many cancers, prostate cancer typically develops slowly over many years. In its early stages, it may not cause any noticeable symptoms, which is why regular screening is so important, particularly for men in higher-risk categories. The cancer cells can remain confined to the prostate gland for a considerable time, a stage known as localised prostate cancer. However, if undetected or untreated, these cancer cells can eventually break through the prostate’s outer membrane and invade nearby tissues or spread to other parts of the body through the bloodstream or lymphatic system, a process known as metastasis. It’s worth noting that not all abnormal growths in the prostate are cancerous, though. Benign prostatic hyperplasia (BPH), for instance, is a common condition in older men where the prostate enlarges but is not cancerous. However, the symptoms of BPH can be similar to those of prostate cancer, which is why proper medical evaluation is crucial for accurate diagnosis.
The development of prostate cancer is a complex process influenced by various factors, including genetics, hormones, environmental exposures, and lifestyle choices. While some risk factors, such as age and family history, cannot be modified, others, like diet and physical activity, can potentially be influenced to reduce risk. Understanding these risk factors and their interplay is crucial for developing effective prevention strategies and identifying individuals who may benefit from more intensive screening.
Risk Factors for Prostate Cancer
The development of prostate cancer, like many complex diseases, is influenced by a multitude of factors. Some of these factors are intrinsic and unchangeable, while others are related to lifestyle choices and environmental exposures. Understanding these risk factors is crucial for identifying individuals at higher risk, implementing appropriate screening protocols, and potentially modifying behaviours to reduce risk where possible. In the context of prostate cancer in Canadian men, several key risk factors have been identified through extensive research and epidemiological studies.
Age
Age stands out as the most significant risk factor for prostate cancer, with the risk increasing substantially as men grow older. The relationship between age and prostate cancer risk is so strong that it’s often said that if a man lives long enough, he will likely develop some form of prostate cancer, even if it’s not clinically significant. In Canada, as in many other countries, prostate cancer is predominantly a disease of older men, with the risk rising sharply after the age of 50.
The reasons for this strong age-related risk are multifaceted. As men age, the cells in their prostate, like cells throughout the body, accumulate genetic mutations. These mutations can occur due to various factors, including natural cellular processes, environmental exposures, and lifestyle factors. Over time, these genetic changes can potentially lead to the uncontrolled cell growth characteristic of cancer. Additionally, the prostate gland tends to enlarge naturally with age, a condition known as benign prostatic hyperplasia (BPH). While BPH itself is not cancerous, the increased cell division associated with this enlargement may increase the chances of cancerous mutations occurring.
It’s important to note that while prostate cancer is rare in men under 40, its incidence begins to rise significantly in the 50-70 age group. By age 80, more than half of all men will have some cancerous cells in their prostate, even if they don’t have clinical symptoms or require treatment. This age-related risk underscores the importance of regular screening for men over 50, or even earlier for those with additional risk factors.
Race and Ethnicity
Race and ethnicity play a significant role in prostate cancer risk, with some groups showing higher incidence rates and more aggressive forms of the disease. In Canada, as in other countries with diverse populations, these racial disparities in prostate cancer risk are evident and of significant concern to healthcare providers and researchers.
Men of African and Caribbean descent, in particular, face a notably higher risk of developing prostate cancer compared to other racial groups. Studies have consistently shown that these men are not only more likely to be diagnosed with prostate cancer but are also more likely to develop the disease at a younger age and to have more aggressive forms of cancer. The reasons for these disparities are not fully understood and are likely due to a complex interplay of genetic, environmental, and socioeconomic factors.
Genetic factors may play a role in these racial differences. Some studies have identified specific genetic variations that are more common in men of African descent and are associated with increased prostate cancer risk. These genetic differences may influence how the body metabolises certain hormones or responds to environmental factors, potentially contributing to the higher risk.
However, it’s crucial to note that genetic factors alone do not fully explain these disparities. Socioeconomic factors, including access to healthcare, dietary habits, and environmental exposures, may also contribute to the increased risk observed in these populations. Additionally, there may be cultural factors that influence health-seeking behaviours and attitudes towards screening, potentially leading to later diagnosis and more advanced disease at the time of detection.
For Canadian men of African or Caribbean descent, awareness of this increased risk is crucial. Healthcare providers often recommend earlier and more frequent screening for these men, typically starting at age 45 or even earlier if there’s a family history of the disease. This proactive approach aims to detect any potential cancers at an earlier, more treatable stage.
Genetic Factors and Family History
Genetic predisposition plays a significant role in prostate cancer risk, with family history being a strong indicator of increased susceptibility. Men who have close relatives (father, brother, or son) diagnosed with prostate cancer are at a higher risk of developing the disease themselves. This familial risk is particularly pronounced if the relative was diagnosed at a young age or if multiple family members have been affected.
The genetic basis of this familial risk is complex and involves multiple genes. While researchers have identified several genes associated with increased prostate cancer risk, the most well-known are the BRCA1 and BRCA2 genes. These genes, which are also associated with increased breast and ovarian cancer risk in women, can significantly elevate a man’s risk of developing prostate cancer when mutated. Men who carry mutations in these genes may develop more aggressive forms of prostate cancer and at younger ages.
Other genes have also been implicated in hereditary prostate cancer risk. For example, mutations in the HOXB13 gene have been associated with early-onset prostate cancer in some families. Additionally, a group of genes involved in DNA repair, including the ATM, CHEK2, and PALB2 genes, have been linked to increased prostate cancer risk when mutated.
It’s important to note that having a genetic predisposition or family history of prostate cancer doesn’t guarantee that an individual will develop the disease. Rather, it indicates an increased risk that warrants closer monitoring and potentially earlier or more frequent screening. For men with a strong family history of prostate cancer, genetic counselling and testing may be recommended to assess their risk more accurately and guide screening and prevention strategies.
The impact of genetic factors on prostate cancer risk underscores the importance of knowing one’s family medical history. Canadian men should be encouraged to discuss their family history with their healthcare providers, as this information can be crucial in determining appropriate screening protocols and risk management strategies.
Diet and Obesity
While age, race, and genetics are uncontrollable risk factors, diet and obesity represent areas where individuals can potentially influence their prostate cancer risk through lifestyle choices. The relationship between diet, obesity, and prostate cancer is complex and continues to be an area of active research, but several key patterns have emerged from epidemiological studies and clinical research.
Diet plays a significant role in overall health and has been linked to prostate cancer risk in various ways. High consumption of red meat and dairy products has been associated with an increased risk of prostate cancer in some studies. These foods are often high in saturated fats and may influence hormone levels in the body, potentially promoting the growth of prostate cancer cells. Additionally, diets high in calcium have been linked to an increased risk, although the exact mechanism is not fully understood. On the other hand, certain dietary patterns and specific foods have been associated with a potential protective effect against prostate cancer. Diets rich in fruits and vegetables, particularly those high in lycopene (found in tomatoes and other red fruits and vegetables), have been linked to a reduced risk of prostate cancer in some studies. Other potentially beneficial foods include those rich in selenium (such as Brazil nuts) and foods containing isoflavones (found in soy products).
Obesity is another significant risk factor for prostate cancer, particularly for more aggressive forms of the disease. Excess body fat, especially abdominal fat, can alter hormone levels in the body, leading to increased production of estrogen and decreased production of testosterone. This hormonal imbalance may create an environment that promotes the growth of prostate cancer cells. Additionally, obesity is associated with chronic inflammation in the body, which may contribute to the development and progression of various cancers, including prostate cancer.
The link between obesity and prostate cancer is particularly relevant in Canada, where obesity rates have been rising in recent decades. According to Statistics Canada, in 2018, 26.8% of Canadian adults were classified as obese, with rates being higher in men compared to women. This trend suggests that a significant proportion of Canadian men may be at increased risk of prostate cancer due to excess body weight.
It’s important to note that while these dietary and lifestyle factors can influence prostate cancer risk, their effects are not absolute. Many men who maintain a healthy diet and weight may still develop prostate cancer, while some men with poor diets or obesity may never develop the disease. However, adopting a healthy lifestyle can have numerous health benefits beyond prostate cancer prevention and is generally recommended for overall well-being.
For Canadian men concerned about their prostate cancer risk, adopting a balanced diet rich in fruits, vegetables, and whole grains, while limiting consumption of red meat and high-fat dairy products, may be beneficial. Maintaining a healthy body weight through a combination of proper nutrition and regular physical activity is also recommended. These lifestyle changes not only have the potential to reduce prostate cancer risk but also offer numerous other health benefits, including reduced risk of heart disease, diabetes, and other cancers.
Signs and Symptoms of Prostate Cancer
Understanding the signs and symptoms of prostate cancer is crucial for early detection and timely intervention. However, it’s important to note that in its early stages, prostate cancer often does not cause any noticeable symptoms. This is one of the reasons why regular screening is so important, particularly for men in higher-risk categories. As the disease progresses, however, various symptoms may begin to manifest. These symptoms can be broadly categorised into changes in urination, changes in sexual function, and general systemic symptoms.
Changes in Urination
Urinary symptoms are often the first noticeable signs of prostate cancer, although it’s important to note that these symptoms can also be caused by non-cancerous conditions such as benign prostatic hyperplasia (BPH). The prostate gland surrounds the urethra, the tube that carries urine from the bladder out of the body. As the prostate enlarges, whether due to cancer or benign growth, it can put pressure on the urethra, leading to various urinary symptoms.
One of the most common urinary symptoms associated with prostate cancer is an increased frequency of urination, particularly at night (nocturia). Men may find themselves needing to urinate more often than usual, sometimes as frequently as every one to two hours. This increased frequency can be disruptive to daily life and sleep patterns, potentially impacting overall quality of life.
Another significant urinary symptom is a reduced flow of urine. Men may notice that their urine stream is weaker than it used to be, or that it takes longer to empty their bladder completely. This reduced flow can be accompanied by a feeling of straining or pushing to initiate urination. Some men may also experience intermittency, where the urine flow stops and starts several times during urination.
A persistent feeling of difficulty emptying the bladder completely is another potential symptom. This sensation can be accompanied by a feeling of urgency to urinate, even shortly after having just done so. This incomplete emptying of the bladder can lead to urinary retention and increase the risk of urinary tract infections.
In some cases, men may notice the presence of blood in their urine, a condition known as hematuria. While this can be alarming, it’s important to note that hematuria can be caused by various conditions, not just prostate cancer. However, any instance of blood in the urine should prompt immediate medical attention to determine the underlying cause.
It’s crucial to emphasise that while these urinary symptoms can be indicative of prostate cancer, they are more commonly caused by benign conditions, particularly in older men. Benign prostatic hyperplasia (BPH), a non-cancerous enlargement of the prostate, is extremely common in older men and can cause many of the same urinary symptoms as prostate cancer. Other conditions such as urinary tract infections or bladder stones can also cause similar symptoms. Therefore, while these symptoms should not be ignored, they should not be cause for immediate alarm. Instead, they should prompt a visit to a healthcare provider for proper evaluation and diagnosis.
Changes in Sexual Function
Prostate cancer can also manifest through changes in sexual function. The prostate gland plays a crucial role in male sexual function, producing seminal fluid that nourishes and transports sperm. As such, problems with the prostate can lead to various sexual symptoms.
One potential symptom is painful ejaculation. Men with prostate cancer may experience discomfort or pain during or immediately after ejaculation. This pain can range from mild to severe and may be felt in the penis, testicles, or the area between the scrotum and rectum (perineum).
A decreased volume of ejaculate is another possible symptom. Men may notice that they produce less semen during ejaculation than they used to. This reduction in ejaculate volume can be gradual and may not be immediately noticeable, but over time it can become more apparent.
Difficulty achieving or maintaining an erection (erectile dysfunction) can also be a symptom of prostate cancer, particularly in its advanced stages. While erectile dysfunction is common in older men and can be caused by various factors, including cardiovascular disease, diabetes, and certain medications, it can also be a result of prostate cancer affecting the nerves or blood vessels involved in achieving an erection.
It’s important to note that many of these sexual symptoms, particularly erectile dysfunction, become more common as men age, regardless of prostate health. However, if these symptoms develop suddenly or worsen rapidly, it’s advisable to seek medical attention. Additionally, treatments for prostate cancer, including surgery and radiation therapy, can sometimes lead to sexual side effects. Therefore, men undergoing treatment for prostate cancer should discuss potential sexual side effects with their healthcare providers and explore options for managing these issues if they arise.
General Systemic Symptoms
As prostate cancer progresses, particularly if it spreads beyond the prostate gland, it can cause a variety of general systemic symptoms. These symptoms are often non-specific and can be indicative of many different health conditions, which is why they should always be evaluated by a healthcare professional.
One of the most common general symptoms of advanced prostate cancer is bone pain. When prostate cancer metastasises, it often spreads to the bones, particularly the spine, pelvis, and ribs. This can cause persistent pain in these areas, which may be worse at night or when resting. The pain can range from a dull ache to a more severe, stabbing sensation. It’s important to note that while bone pain can be a symptom of metastatic prostate cancer, it can also be caused by many other conditions, including arthritis or osteoporosis, which are common in older men.
Fatigue is another potential symptom of advanced prostate cancer. This is not just ordinary tiredness that can be relieved by rest, but a persistent feeling of exhaustion that interferes with daily activities. Cancer-related fatigue can be caused by the cancer itself, as the body expends energy fighting the disease, or it can be a side effect of cancer treatments. However, fatigue is a non-specific symptom that can be caused by numerous health conditions, as well as lifestyle factors such as poor sleep or stress.
Unexplained weight loss can also be a sign of advanced prostate cancer. If a man loses a significant amount of weight without trying to do so through diet or exercise, it could be a cause for concern. Cancer cells can alter metabolism and increase the body’s energy demands, leading to weight loss even when eating habits haven’t changed. However, like fatigue, unexplained weight loss can be a symptom of many different health conditions and should always be evaluated by a healthcare provider.
Lower extremity swelling, particularly in the legs and feet, can occur in advanced stages of prostate cancer. This swelling, known as edema, can be caused by the cancer obstructing lymph nodes or blood vessels, leading to fluid accumulation in the tissues. However, edema can also be caused by many other conditions, including heart failure, kidney disease, or liver problems, which are not uncommon in older adults.
Some men with advanced prostate cancer may experience numbness or tingling in their lower extremities. This can occur if the cancer spreads to the spine and puts pressure on the nerves that control sensation in the legs and feet. However, numbness and tingling can also be symptoms of many other conditions, including diabetes, which is common in older adults.
Finally, some men with prostate cancer may experience a general feeling of being unwell, often described as malaise. This can manifest as a lack of energy, decreased appetite, or a general sense that something isn’t right with their health. While this symptom is non-specific, any persistent feeling of being unwell should be evaluated by a healthcare provider.
It’s crucial to emphasise that many of these general symptoms, while potentially indicative of advanced prostate cancer, are more commonly caused by other health conditions, particularly in older adults. Furthermore, early-stage prostate cancer often causes no symptoms at all. This underscores the importance of regular prostate cancer screening for men at risk, as early detection can lead to more effective treatment and better outcomes.
Screening and Diagnosis
Early detection of prostate cancer is crucial for effective treatment and improved outcomes. In Canada, as in many countries, there has been ongoing debate about the best approach to prostate cancer screening. While screening can help detect cancer at an early, more treatable stage, it can also lead to overdiagnosis and overtreatment of slow-growing cancers that may never cause symptoms or shorten a man’s life. Understanding the screening process, its benefits, and potential drawbacks is essential for Canadian men making decisions about their prostate health.
Prostate-Specific Antigen (PSA) Test
The primary screening tool for prostate cancer is the prostate-specific antigen (PSA) test. PSA is a protein produced by the prostate gland, and elevated levels in the blood can indicate the presence of prostate cancer. However, PSA levels can also be elevated due to non-cancerous conditions such as benign prostatic hyperplasia (BPH) or prostatitis, leading to false-positive results.
In Canada, there is no national screening program for prostate cancer, and recommendations for PSA testing vary. The Canadian Task Force on Preventive Health Care recommends against PSA screening for men under 55 and over 70 years of age. For men aged 55-69, the task force suggests not routinely screening for prostate cancer with the PSA test. However, they acknowledge that some men in this age group may place high value on the small potential reduction in the risk of death from prostate cancer and are willing to risk the potential harms associated with screening. In these cases, the decision to undergo PSA screening should be made on an individual basis after a thorough discussion with a healthcare provider about the potential benefits and harms.
It’s important to note that PSA levels can be influenced by various factors, including age, prostate size, and certain medications. Therefore, a single elevated PSA result does not necessarily indicate cancer. If an elevated PSA level is found, additional tests may be recommended to determine the cause.
Digital Rectal Examination (DRE)
The digital rectal examination (DRE) is another screening tool for prostate cancer. During this examination, a healthcare provider inserts a gloved, lubricated finger into the rectum to feel the prostate gland for any abnormalities in size, shape, or texture. While the DRE can detect abnormalities in the prostate, it has limitations. It can only assess the posterior and lateral portions of the prostate, and small tumours may not be palpable.
In Canada, the DRE is often used in conjunction with the PSA test for prostate cancer screening. However, like the PSA test, there is debate about its effectiveness as a standalone screening tool. Some guidelines suggest that the DRE should not be used as a primary screening test for prostate cancer due to lack of evidence of its effectiveness in reducing prostate cancer mortality.
Prostate Biopsy
If screening tests suggest the possibility of prostate cancer, the next step is usually a prostate biopsy. This procedure involves taking small samples of tissue from the prostate gland for examination under a microscope. The most common method is a transrectal ultrasound-guided biopsy, where an ultrasound probe is inserted into the rectum to visualise the prostate while a thin needle is used to collect tissue samples.
Prostate biopsies are typically performed on an outpatient basis and carry some risks, including bleeding and infection. It’s important to note that while a biopsy is the most definitive way to diagnose prostate cancer, it can sometimes miss cancer if the sampled areas do not contain cancerous cells. In some cases, if initial biopsy results are negative but suspicion of cancer remains high, additional biopsies or other imaging studies may be recommended.
Advanced Imaging Techniques
In recent years, advanced imaging techniques have been increasingly used in the diagnosis and staging of prostate cancer. Multiparametric magnetic resonance imaging (mpMRI) has emerged as a valuable tool in prostate cancer diagnosis. It can provide detailed images of the prostate and help identify suspicious areas that may require biopsy. In some cases, MRI can be used to guide biopsy procedures, potentially improving the accuracy of sampling.
Positron emission tomography (PET) scans, particularly those using prostate-specific membrane antigen (PSMA) tracers, are also becoming more widely used, especially for detecting the spread of prostate cancer to other parts of the body. These advanced imaging techniques can provide more accurate information about the extent and aggressiveness of the cancer, helping to guide treatment decisions.
Treatment Options
When prostate cancer is diagnosed, the choice of treatment depends on several factors, including the stage and grade of the cancer, the patient’s age and overall health, and personal preferences. In Canada, as in many countries, there is a range of treatment options available, from active surveillance for low-risk cancers to more aggressive interventions for advanced disease. Understanding these options is crucial for Canadian men facing a prostate cancer diagnosis.
Active Surveillance
For men with low-risk, early-stage prostate cancer, active surveillance may be recommended. This approach involves closely monitoring the cancer through regular PSA tests, digital rectal exams, and periodic biopsies, without immediately pursuing active treatment. The goal is to avoid unnecessary treatment and its potential side effects while still being able to intervene if the cancer shows signs of progression. Active surveillance is particularly appropriate for older men or those with other serious health conditions, for whom the risks of treatment may outweigh the benefits. It’s also suitable for men with very slow-growing prostate cancer that are unlikely to cause problems during their lifetime.
Surgery
Radical prostatectomy, the surgical removal of the entire prostate gland and some surrounding tissue, is a common treatment option for localised prostate cancer. This procedure can be performed through traditional open surgery or using minimally invasive techniques such as laparoscopic or robotic-assisted surgery.
In Canada, robotic-assisted prostatectomy has become increasingly available in recent years, although access may vary depending on the region. This technique offers potential benefits such as smaller incisions, less blood loss, and potentially faster recovery times. However, the long-term outcomes in terms of cancer control and side effects are generally similar to those of traditional open surgery.
The main potential side effects of radical prostatectomy include urinary incontinence and erectile dysfunction. These side effects can significantly impact quality of life, and their likelihood and severity can vary depending on factors such as the patient’s age, preoperative function, and the surgeon’s experience.
Radiation Therapy
Radiation therapy is another primary treatment option for prostate cancer. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy). External beam radiation therapy involves directing high-energy x-rays at the prostate from outside the body. Modern techniques such as intensity-modulated radiation therapy (IMRT) and image-guided radiation therapy (IGRT) allow for more precise targeting of the cancer while minimising damage to surrounding healthy tissues.
Brachytherapy involves placing small radioactive seeds directly into the prostate gland. This can be done as a permanent implant (low-dose-rate brachytherapy) or as a temporary implant (high-dose-rate brachytherapy). Brachytherapy may be used alone for early-stage cancers or in combination with external beam radiation for more advanced cases.
Radiation therapy can cause side effects such as urinary problems, bowel issues, and erectile dysfunction. These side effects can develop during treatment or appear months to years after treatment has ended. However, modern radiation techniques have helped reduce the severity and frequency of these side effects.
Hormone Therapy
Hormone therapy, also known as androgen deprivation therapy (ADT), is a treatment that reduces levels of male hormones (androgens) in the body or blocks their effects on prostate cancer cells. This can be achieved through medications that lower testosterone levels or block testosterone from acting on prostate cancer cells, or through surgical removal of the testicles (orchiectomy).
Hormone therapy is often used in combination with radiation therapy for intermediate or high-risk localised prostate cancer. It’s also a standard treatment for metastatic prostate cancer. While hormone therapy can be very effective in controlling prostate cancer growth, it can cause significant side effects, including hot flashes, loss of libido, erectile dysfunction, bone loss, and increased risk of cardiovascular problems.
In Canada, various forms of hormone therapy are available, including luteinizing hormone-releasing hormone (LHRH) agonists and antagonists, anti-androgens, and newer hormonal agents such as abiraterone and enzalutamide. The choice of hormonal therapy depends on the stage of the cancer, the patient’s overall health, and whether the cancer has become resistant to initial hormone treatments.
Chemotherapy
Chemotherapy is typically reserved for advanced prostate cancer that has spread beyond the prostate and is no longer responding to hormone therapy. The most commonly used chemotherapy drug for prostate cancer is docetaxel, although other drugs may also be used.
In Canada, chemotherapy for prostate cancer is usually administered in specialised cancer centres. While it can help control cancer growth and alleviate symptoms in some men with advanced disease, it can also cause significant side effects such as fatigue, nausea, hair loss, and increased risk of infections.
The Importance of Multidisciplinary Care
In Canada, the treatment of prostate cancer increasingly involves a multidisciplinary approach, with input from urologists, radiation oncologists, medical oncologists, and other specialists. This team-based approach ensures that patients receive comprehensive care that considers all available treatment options.
Moreover, the psychological impact of a prostate cancer diagnosis and treatment should not be underestimated. Many cancer centres in Canada offer support services, including counselling and support groups, to help patients and their families cope with the emotional aspects of the disease.
The choice of treatment for prostate cancer is highly individualised and should take into account not only the characteristics of the cancer but also the patient’s overall health, life expectancy, and personal preferences. Canadian men diagnosed with prostate cancer should engage in thorough discussions with their healthcare providers to understand all available options and make informed decisions about their care.
Living with Prostate Cancer: Quality of Life Considerations
A diagnosis of prostate cancer and its subsequent treatment can have profound effects on a man’s quality of life. While medical interventions focus on controlling the cancer, it’s equally important to address the physical, emotional, and social impacts of the disease and its treatment. For Canadian men living with prostate cancer, understanding these quality of life issues and knowing how to address them is crucial for maintaining overall well-being.
Physical Effects and Management
The physical side effects of prostate cancer treatment can be significant and may persist long after treatment has ended. Two of the most common and impactful side effects are urinary incontinence and erectile dysfunction.
Urinary incontinence, or the inability to control urine flow, is a common side effect of both surgery and radiation therapy for prostate cancer. The severity can range from occasional leakage to complete loss of bladder control. This can have a significant impact on daily life, affecting work, social activities, and intimate relationships. Management strategies for urinary incontinence include:
- Pelvic floor exercises (Kegel exercises) to strengthen the muscles that control urination
- Bladder training techniques to improve control
- Lifestyle modifications, such as limiting caffeine and alcohol intake
- Use of incontinence products like pads or protective underwear
- Medications to improve bladder control
- In severe cases, surgical interventions such as artificial urinary sphincter implantation
Erectile dysfunction (ED) is another common side effect of prostate cancer treatment, particularly after surgery or radiation therapy. The nerves that control erections can be damaged during treatment, leading to difficulty achieving or maintaining an erection. This can have a significant impact on a man’s self-esteem and intimate relationships. Management options for ED include:
- Oral medications such as sildenafil (Viagra), tadalafil (Cialis), or vardenafil (Levitra)
- Vacuum erection devices
- Intracavernosal injections
- Penile implants
It’s important to note that recovery of urinary and sexual function can take time, sometimes up to
two years after treatment. Patience and ongoing communication with healthcare providers are crucial during this recovery period.
Other physical side effects of prostate cancer treatment can include fatigue, hot flashes (particularly with hormone therapy), bone loss, and changes in body composition. These effects can be managed through a combination of medication, lifestyle modifications, and supportive care. For example, weight-bearing exercises and calcium supplements can help mitigate bone loss, while a balanced diet and regular physical activity can help manage fatigue and body composition changes.
Emotional and Psychological Impact
The emotional and psychological impact of prostate cancer can be profound. Men may experience a range of emotions, including fear, anxiety, depression, and anger. The uncertainty of the disease course, concerns about treatment side effects, and changes in self-image and sexuality can all contribute to psychological distress.
In Canada, psychosocial support is increasingly recognised as an integral part of comprehensive cancer care. Many cancer centres offer counselling services, support groups, and other psychosocial interventions to help patients and their families cope with the emotional aspects of prostate cancer. These services can provide valuable emotional support, practical coping strategies, and opportunities to connect with others facing similar challenges.
It’s important for men with prostate cancer to be aware that feelings of distress are normal and that seeking help is a sign of strength, not weakness. Healthcare providers should routinely screen for psychological distress and refer patients to appropriate support services when needed.
Impact on Relationships and Intimacy
Prostate cancer and its treatment can have a significant impact on relationships, particularly intimate partnerships. Changes in sexual function, urinary issues, and the emotional stress of dealing with cancer can all strain relationships. Open communication between partners is crucial for navigating these challenges.
Many Canadian cancer centres offer counselling services specifically focused on sexual health and intimacy issues related to prostate cancer. These services can help couples explore alternative ways of expressing intimacy and maintaining closeness, even in the face of physical changes.
It’s also important to note that prostate cancer can affect family dynamics more broadly. Adult children may find themselves in caregiving roles, and family routines may need to be adjusted to accommodate treatment schedules and recovery periods. Family counselling or support groups for family members can be valuable resources in these situations.
Work and Financial Considerations
For many Canadian men, a prostate cancer diagnosis can have significant implications for work and finances. Treatment schedules may require time off work, and side effects may impact job performance. Some men may need to reduce their work hours or even retire earlier than planned.
Canadian employment laws provide some protections for workers with serious illnesses, including job-protected leave for medical treatments. However, the specifics can vary by province, and not all workers may be eligible for these protections. It’s important for men with prostate cancer to understand their rights and discuss their situation with their employers.
Financial stress can be a significant concern for many prostate cancer patients. While the Canadian healthcare system covers many cancer-related medical expenses, there can still be out-of-pocket costs for medications, travel to treatment centres, and supportive care services. Additionally, reduced income due to time off work can strain household finances.
Various organisations in Canada offer financial assistance programs for cancer patients. These can include help with medication costs, travel expenses, or general financial support. Social workers at cancer centres can often provide information about these programs and assist with applications.
Lifestyle and Self-Care
Adopting a healthy lifestyle can play a crucial role in managing the effects of prostate cancer and its treatment. While lifestyle changes can’t cure prostate cancer, they may help manage side effects, improve overall health, and potentially reduce the risk of cancer recurrence or progression.
Key aspects of a healthy lifestyle for men with prostate cancer include:
- Regular physical activity: Exercise can help manage fatigue, improve mood, maintain bone and muscle strength, and potentially improve cancer outcomes. The Canadian Society for Exercise Physiology recommends at least 150 minutes of moderate to vigorous aerobic activity per week for adults, along with strength training exercises at least twice a week.
- Healthy diet: While no specific diet has been proven to cure prostate cancer, a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health. Some studies suggest that a diet low in animal fats and high in plant-based foods may be beneficial for men with prostate cancer.
- Stress management: Techniques such as meditation, yoga, or deep breathing exercises can help manage stress and improve overall well-being.
- Adequate sleep: Good sleep hygiene is important for managing fatigue and supporting overall health.
- Avoiding harmful substances: Quitting smoking and limiting alcohol intake can support overall health and potentially improve cancer outcomes.
It’s important for men to discuss any planned lifestyle changes with their healthcare providers to ensure they are safe and appropriate for their individual situation.
Survivorship Care
As more men survive prostate cancer, there is increasing focus on long-term survivorship care. In Canada, survivorship care plans are becoming more common. These plans provide a summary of a patient’s cancer diagnosis and treatment, a schedule for follow-up care, information about potential long-term side effects, and recommendations for healthy living. Long-term follow-up care for prostate cancer survivors typically includes regular PSA tests to monitor for any signs of cancer recurrence, as well as screening for potential late effects of treatment. This may include bone density scans to monitor for osteoporosis, particularly in men who have undergone long-term hormone therapy.
Survivorship care also involves monitoring for and managing any ongoing side effects of treatment, as well as addressing the psychosocial aspects of living as a cancer survivor. This can include helping survivors navigate the emotional challenges of transitioning from active treatment to long-term follow-up care, addressing fears of cancer recurrence, and supporting the resumption of normal life activities.
The Role of Support Networks
Support networks can play a crucial role in helping men navigate life with prostate cancer. These networks can include family and friends, healthcare providers, support groups, and community organisations. In Canada, numerous organisations provide support and resources for men with prostate cancer and their families. These include:
- Prostate Cancer Canada: A national organisation that provides information, support services, and advocacy for men with prostate cancer and their families.
- Canadian Cancer Society: Offers a range of support services, including a peer support program that connects cancer patients with trained volunteers who have had similar cancer experiences.
- Local support groups: Many communities across Canada have prostate cancer support groups where men can share experiences and information with others facing similar challenges.
- Online communities: Various online forums and social media groups provide platforms for men with prostate cancer to connect and share information.
Engaging with these support networks can provide valuable emotional support, practical information, and a sense of community for men dealing with prostate cancer.
It’s important to emphasise that while prostate cancer remains a serious health concern, there is reason for optimism. With ongoing advances in prevention, early detection, treatment, and supportive care, the outlook for Canadian men facing prostate cancer continues to improve. By staying informed, engaging in open communication with healthcare providers, and accessing available support resources, Canadian men can navigate the challenges of prostate cancer with confidence and hope.
Ultimately, the story of prostate cancer in Canada is one of resilience, progress, and community. It’s a story of researchers working tirelessly to unlock the secrets of this disease, of healthcare providers dedicating themselves to providing the best possible care, of families and communities rallying around those affected, and of countless men facing their diagnosis with courage and determination. As we continue to write this story together, we move ever closer to a future where prostate cancer no longer poses a significant threat to the health and wellbeing of Canadian men.
-
Peanut-Free Classrooms
As a physician, I am often approached by parents seeking guidance on how to ensure their children’s safety and well-being in the classroom environment. In this comprehensive article, we will delve into the complexities of food allergies, with a particular focus on peanut allergies, and explore the measures that can be taken to create a safe and inclusive learning environment for all students.
Peanut allergies are increasingly prevalent, emerging as one of the most common food allergies among children in Canada and around the world. The ubiquity of peanuts and peanut-containing products in our daily lives, coupled with the potential severity of allergic reactions, has led to heightened awareness and concern, especially in school settings. As we navigate this landscape, it is crucial to understand the nature of peanut allergies, their potential impact on affected individuals, and the strategies that can be employed to mitigate risks while fostering a supportive and understanding community.
The immune system, typically our body’s stalwart defender against harmful pathogens, sometimes misidentifies certain proteins found in peanuts as potential threats. This misidentification triggers an immune response that can manifest in a variety of symptoms, ranging from mild discomfort to life-threatening anaphylaxis. It is this unpredictability and the potential severity of reactions that necessitates a comprehensive approach to managing peanut allergies in school environments. As we delve deeper into this topic, we will explore the physiological mechanisms underlying allergic reactions, the various ways in which exposure can occur, and the steps that can be taken to create a safe and inclusive learning environment for all students.
The prevalence of peanut allergies has been on the rise in recent decades, with studies indicating a significant increase in diagnosed cases among children. While the exact reasons for this upward trend remain a subject of ongoing research, several theories have been proposed, including changes in dietary habits, environmental factors, and evolving hygiene practices. Regardless of the underlying causes, the reality is that many classrooms now include one or more students with peanut allergies, necessitating a thoughtful and proactive approach to allergy management.
As we consider the impact of peanut allergies on the school environment, it is important to recognize that the issue extends beyond the affected individuals themselves. The entire school community – including teachers, administrators, food service staff, and fellow students – plays a role in creating a safe and supportive atmosphere. This collective responsibility underscores the importance of education, communication, and collaboration in addressing the challenges posed by food allergies in the classroom.
One of the primary considerations for schools in managing peanut allergies is the implementation of policies regarding the presence of peanuts and peanut-containing products on school premises. Many educational institutions have opted to establish nut-free or nut-aware policies, which restrict or prohibit the consumption of peanuts and tree nuts within the school environment. These policies can take various forms, ranging from complete bans on nut products to designated nut-free zones within the school. The specific approach adopted by a school often depends on factors such as the prevalence of allergies within the student body, the age of the students, and the physical layout of the school facilities. It is also important to note that while many schools have implemented nut-free or nut-aware policies, the specific guidelines can vary significantly from one institution to another. Some schools may enforce a blanket ban on all nut products, while others may adopt a more nuanced approach that allows for controlled consumption in certain areas. Given this variability, it is crucial for parents and caregivers to consult directly with school officials to understand the specific policies and procedures in place at their child’s educational institution. This proactive communication ensures that all parties are aware of the expectations and can work together to create a safe and inclusive environment for all students.
The implementation of nut-free or nut-aware policies in schools is not without its challenges. Critics argue that such measures may create a false sense of security, potentially leading to complacency in other aspects of allergy management. Additionally, concerns have been raised about the nutritional impact of restricting certain foods, particularly for students who rely on nut-based products as a source of protein or other essential nutrients. These valid concerns underscore the importance of adopting a balanced and comprehensive approach to allergy management that goes beyond simply banning certain foods.
As we consider the various strategies for managing peanut allergies in the school environment, it is essential to recognize that no single approach can guarantee absolute safety. Instead, a multi-faceted strategy that combines policy measures, education, and individual management plans is often the most effective way to address the complex challenges posed by food allergies. This holistic approach not only helps to mitigate the risks associated with allergic reactions but also fosters a culture of understanding and support within the school community.
One crucial aspect of managing peanut allergies in the school setting is the development and implementation of individualized allergy action plans. These plans, typically created in collaboration with the student’s healthcare provider, outline specific steps to be taken in the event of an allergic reaction. These plans may include details such as the student’s known allergens, typical symptoms of a reaction, emergency contact information, and instructions for administering medication such as epinephrine auto-injectors. By having these plans in place and ensuring that relevant staff members are familiar with their contents, schools can be better prepared to respond quickly and effectively in the event of an allergic emergency.
Education plays a pivotal role in creating a safe and supportive environment for students with peanut allergies. This education should extend to all members of the school community, including students, teachers, administrators, and support staff. For students, age-appropriate instruction on food allergies can help foster empathy and understanding, encouraging them to be mindful of their classmates’ needs. This education might include lessons on the basics of food allergies, the importance of not sharing food, and what to do if they suspect a classmate is having an allergic reaction. For school staff, comprehensive training on allergy management is essential. This training should cover topics such as recognizing the signs and symptoms of an allergic reaction, understanding how to use epinephrine auto-injectors, and implementing strategies to prevent accidental exposure to allergens. By equipping staff members with this knowledge, schools can create a safer environment for students with allergies and ensure that appropriate action is taken in the event of an emergency.
In addition to education and training, schools can implement a variety of practical measures to reduce the risk of accidental exposure to peanuts and other allergens. These measures might include establishing protocols for cleaning surfaces where food is consumed, implementing hand-washing procedures before and after meals, and creating designated eating areas for students with allergies. Some schools have also adopted policies that require students to eat only food provided from home, reducing the risk of exposure to unknown allergens through shared or traded food items.
The role of communication in managing peanut allergies in the school environment cannot be overstated. Open and ongoing dialogue between parents, school administrators, teachers, and healthcare providers is crucial for ensuring that all parties are aligned in their approach to allergy management. This communication should begin well before the start of the school year, allowing ample time for the development and implementation of appropriate policies and procedures.
Parents of children with peanut allergies should take a proactive approach in communicating with their child’s school. This may involve scheduling meetings with teachers and administrators to discuss their child’s specific needs, providing detailed information about the nature and severity of the allergy, and collaborating on the development of an individualized allergy action plan. By fostering this open line of communication, parents can help ensure that their child’s needs are understood and addressed within the school environment.
Equally important is the communication between the school and the broader parent community. Schools should strive to keep all parents informed about allergy-related policies and procedures, explaining the rationale behind these measures and soliciting support and cooperation. This might involve sending out informational letters, hosting parent information sessions, or including allergy-related information in school newsletters and on the school website. By engaging the entire school community in this way, schools can foster a culture of understanding and shared responsibility for student safety.
Another important consideration in the management of peanut allergies in schools is the psychological and emotional impact on affected students. Children with food allergies may experience anxiety, social isolation, or bullying related to their condition. Schools play a crucial role in addressing these challenges by fostering a supportive and inclusive environment. This might involve implementing anti-bullying policies that specifically address food allergy-related teasing or exclusion, providing counselling services for students struggling with anxiety related to their allergies, and promoting inclusivity in all school activities and events.
As we navigate the complexities of managing peanut allergies in the school environment, it is crucial to maintain a balance between safety and inclusivity. While the primary goal is undoubtedly to protect students with allergies from potentially life-threatening reactions, it is also important to ensure that these students are able to fully participate in all aspects of school life. This might involve finding creative solutions to include students with allergies in classroom activities, field trips, and social events that might otherwise pose a risk. For example, rather than excluding a student with a peanut allergy from a cooking class, the teacher might modify the lesson plan to use alternative ingredients that are safe for all students. Similarly, when planning field trips or other off-site activities, schools should work closely with parents and venues to ensure that appropriate accommodations are in place to allow all students to participate safely. By working together – parents, educators, healthcare providers, and the broader community – we can create school environments that not only protect students with peanut allergies from potential harm but also empower them to thrive and fully participate in all aspects of school life. Through education, communication, and a commitment to inclusivity, we can ensure that all students, regardless of their allergies or other health conditions, have the opportunity to learn, grow, and succeed in a safe and supportive environment.
As we begin this new school year, let us recommit ourselves to the principles of safety, inclusivity, and mutual respect. Let us continue to strive for solutions that balance the needs of all students while prioritizing the well-being of those with food allergies. And let us remember that in addressing the challenges posed by peanut allergies in schools, we are not just protecting individual students – we are building stronger, more compassionate communities that value the health and safety of all their members. As we move forward, may we approach this task with empathy, creativity, and an unwavering commitment to ensuring that every child has the opportunity to learn and grow in a safe and supportive environment.
-
Back-to-School Health Tips
Back-to-school is a time that can be as thrilling as it is nerve-wracking, particularly when one considers the broad spectrum of health concerns that accompany this pivotal period in the academic calendar, whether one’s child is stepping into a classroom for the very first time, navigating the often tumultuous waters of adolescence, or embarking on the independent journey of higher education. The importance of fostering and maintaining good health practices cannot be overstated, as these habits are not only crucial for academic success, but also for the overall well-being of students, ensuring they are equipped to handle the physical, emotional, and mental challenges that inevitably arise throughout the school year.
Physical Health and Nutrition
For younger children, who are still developing their immune systems and establishing their foundational health habits, ensuring that they receive proper nutrition is one of the most critical steps parents can take. A balanced diet, rich in fruits, vegetables, whole grains, and lean proteins, provides the essential nutrients that are necessary for growth, cognitive function, and energy levels. It is important to recognize that what children consume during their formative years can have long-lasting effects on their health, including their ability to focus in school, their mood, and their overall energy levels. Packing a lunch that is both nutritious and appealing to young taste buds can be a challenge, but it is essential to include items that are high in fibre, low in sugar, and free from excessive processed ingredients. Encouraging children to participate in the preparation of their own lunches can also be a helpful strategy, as it fosters a sense of independence and teaches them valuable lessons about healthy eating habits that will serve them well as they grow older.
As children grow into teenagers, the focus on physical health becomes even more important, given that this is a period of rapid growth and development, both physically and mentally. Teenagers require a higher caloric intake to support their increased energy needs, but it is equally important to ensure that these calories come from nutritious sources rather than junk food or sugary beverages. Adolescents are particularly susceptible to developing unhealthy eating habits, especially when they begin to experience the pressures of social conformity and body image issues. It is vital to educate teenagers about the importance of maintaining a balanced diet that includes a variety of nutrients, and to encourage them to make healthier choices, even when they are on the go. Moreover, for those who participate in sports or other physical activities, proper nutrition becomes even more crucial, as it directly impacts their performance, endurance, and recovery times. Hydration is another key aspect of physical health that is often overlooked; ensuring that teenagers drink enough water throughout the day is essential, especially during the warmer months or after physical exertion.
For college and university students, who are often living away from home for the first time and navigating the complexities of adulthood, maintaining a healthy diet can be particularly challenging. The newfound freedom of being able to make their own food choices, combined with the stress and time constraints of academic life, can lead to poor eating habits, such as skipping meals, relying on fast food, or indulging in late-night snacks. However, it is crucial for students to understand that their dietary choices have a direct impact on their ability to concentrate, retain information, and perform well in their studies. Meal planning and preparation can be a valuable skill for college students to develop, as it not only helps them save money, but also ensures that they are consuming balanced meals that provide the energy and nutrients needed to support their academic and physical endeavours. Additionally, students should be mindful of the importance of regular physical activity, as it not only helps to maintain a healthy weight, but also has been shown to improve mood, reduce stress, and enhance cognitive function, all of which are vital for success in higher education.
Mental Health and Emotional Well-Being
While physical health is undeniably important, it is equally crucial to address the mental and emotional well-being of students, as this is a key factor in their overall health and academic performance. For younger children, the transition back to school can be a source of anxiety, particularly if they are entering a new environment or facing the challenges of making new friends. Parents and caregivers should be attentive to any signs of stress or anxiety in their children, such as changes in behaviour, sleep patterns, or appetite. Encouraging open communication about their feelings and providing reassurance can help alleviate some of the anxieties associated with returning to school. Additionally, establishing a consistent routine, including a regular bedtime and a structured homework schedule, can provide a sense of stability and predictability that is comforting for children.
Teenagers, who are often dealing with the pressures of academic performance, social dynamics, and the onset of puberty, may experience a heightened sense of stress and anxiety during the back-to-school period. It is important for parents and educators to recognize that teenagers are particularly vulnerable to mental health issues, such as depression and anxiety, which can be exacerbated by the demands of school and extracurricular activities. Providing teenagers with the tools to manage stress, such as mindfulness techniques, time management skills, and access to counselling services, can be invaluable in helping them navigate this challenging period. Moreover, fostering a supportive and open environment at home, where teenagers feel comfortable discussing their concerns without fear of judgment, is crucial for their emotional well-being.
For college and university students, the transition to higher education often comes with its own set of mental health challenges, including the stress of academic expectations, the pressure to fit in socially, and the adjustment to living away from home. It is not uncommon for students to experience feelings of loneliness, homesickness, or overwhelm, particularly during the first few months of college. It is important for students to be proactive about their mental health by seeking out resources available on campus, such as counselling services, mental health workshops, and peer support groups. Additionally, maintaining a healthy work-life balance, setting realistic academic goals, and prioritizing self-care are all essential strategies for managing stress and preventing burnout. Regular physical activity, adequate sleep, and a balanced diet are also important components of mental health, as they contribute to overall well-being and help students cope with the demands of academic life.
Sleep and Rest
Another critical aspect of health that is often overlooked, particularly in the context of the back-to-school transition, is the importance of sleep and rest. For younger children, who are still developing both physically and cognitively, adequate sleep is essential for growth, learning, and overall well-being. Establishing a consistent bedtime routine, which includes winding down with quiet activities such as reading or listening to calming music, can help children transition more easily into sleep. It is also important to ensure that the sleep environment is conducive to rest, which means keeping the bedroom dark, cool, and free from distractions such as electronic devices.
Teenagers, who often experience a natural shift in their sleep-wake cycle during adolescence, may find it challenging to get the recommended amount of sleep, particularly when they are juggling academic responsibilities, extracurricular activities, and social commitments. However, chronic sleep deprivation can have serious consequences for both physical and mental health, including impaired concentration, mood swings, and a weakened immune system. Encouraging teenagers to establish a regular sleep schedule, limit caffeine intake, and create a relaxing bedtime routine can help them get the rest they need to function at their best.
For college and university students, who are often balancing demanding academic workloads with social activities and part-time jobs, getting enough sleep can be particularly challenging. However, sleep is crucial for cognitive function, memory consolidation, and overall health. Students should be encouraged to prioritize sleep by creating a sleep-friendly environment, avoiding all-nighters, and managing their time effectively to ensure they have adequate rest. Additionally, taking short naps during the day, when needed, can help students recharge and maintain their energy levels.
Preventing Illness and Building Immunity
As students of all ages return to school, they are inevitably exposed to a variety of germs and viruses, making illness prevention a key concern for parents, educators, and students alike. For younger children, who are still building their immune systems, it is important to teach them good hygiene practices, such as washing their hands regularly, covering their mouths when they cough or sneeze, and avoiding close contact with sick individuals. Parents can also help boost their children’s immunity by ensuring they get enough sleep, eat a balanced diet, and stay physically active.
Teenagers and college students, who are often in close contact with others in classrooms, dormitories, and social settings, should also be vigilant about hygiene and illness prevention. In addition to practising good hygiene, getting vaccinated against common illnesses, such as the flu, can help reduce the risk of infection. Maintaining a healthy lifestyle, including regular exercise, a balanced diet, and adequate sleep, is also important for supporting the immune system and preventing illness.
Preparing for the Academic Year
Finally, it is important to consider the overall preparation for the academic year, which includes not only physical and mental health, but also practical considerations such as school supplies, transportation, and time management. For younger children, having the right school supplies, such as notebooks, pencils, and backpacks, can help them feel prepared and confident as they start the new school year. Parents should also ensure that their children have a safe and reliable means of transportation to and from school, whether it be walking, biking, or taking the bus.
Teenagers, who may have more complex academic schedules and responsibilities, should be encouraged to take an active role in organizing their school supplies, planning their daily routines, and managing their time effectively. This may include setting up a study schedule, organizing their homework and assignments, and ensuring they have the necessary tools and resources to succeed.
For college and university students, preparation for the academic year may involve setting up their living spaces, purchasing textbooks and other materials, and planning their course schedules. It is also important for students to familiarize themselves with the resources available on campus, such as academic advising, tutoring services, and student health services, which can be invaluable in helping them navigate the challenges of higher education.
-
International Overdose Awareness Day 2024
Every year on August 31, communities around the world come together to observe International Overdose Awareness Day (IOAD), the largest annual campaign dedicated to ending overdose, remembering those who have lost their lives to this epidemic without stigma, and acknowledging the profound grief experienced by the family and friends left behind. The theme for IOAD 2024, “Together we can,” underscores the tremendous power of community when everyone stands united in the face of this ongoing public health crisis.
The opioid overdose epidemic has had a devastating impact in Canada, with a staggering 5,975 lives lost in 2023 alone. Tragically, around 30 percent of these deaths occurred among individuals aged 30 to 39 years, highlighting the disproportionate toll this crisis has taken on young adults in the prime of their lives. Behind each of these statistics lies a unique individual with hopes, dreams, and loved ones who are now left to grapple with the immeasurable pain of their absence.
Compounding the tragedy of these losses is the pervasive stigma that continues to surround substance use disorders and overdose deaths. This stigma, rooted in misunderstanding and often perpetuated by societal attitudes and media portrayals, can have profound and far-reaching consequences for both individuals struggling with addiction and those who have lost loved ones to overdose. For those actively battling substance use disorders, stigma can serve as a formidable barrier to seeking help and accessing the life-saving treatments and support services they so desperately need. The fear of judgment, discrimination, and social ostracization can lead individuals to conceal their struggles, isolating themselves from the very resources and networks that could offer a path to recovery. This isolation not only exacerbates the psychological and emotional distress associated with addiction but also increases the risk of overdose, as individuals may be more likely to use substances alone and without access to harm reduction measures like naloxone.
The stigma surrounding overdose deaths can also have a profound impact on the mental health and well-being of those left behind. Family members and friends who have lost loved ones to overdose often find themselves navigating a complex landscape of grief, guilt, and shame, their pain compounded by societal attitudes that may blame the individual for their own death or view addiction as a moral failing rather than a medical condition. This stigma can make it difficult for those who are grieving to openly discuss their loss, access bereavement support services, and find the compassion and understanding they need to heal.
Challenging and dismantling the stigma surrounding opioid overdose is a critical step in addressing this public health crisis and supporting those affected by it. This requires a multi-faceted approach that includes public education campaigns to raise awareness about the realities of substance use disorders, the expansion of evidence-based treatment and harm reduction services, and the cultivation of compassionate, non-judgmental attitudes within communities.
Events like International Overdose Awareness Day play a vital role in this process, providing a platform for individuals and communities to come together in remembrance, solidarity, and action. By openly discussing the impact of overdose, sharing stories of loss and recovery, and advocating for policy changes that prioritize public health and harm reduction, we can work to create a society that treats addiction as a medical issue rather than a moral one and provides the support and resources needed to prevent further loss of life.
As we approach IOAD 2024, let us embrace the theme of “Together we can” and recognize the collective power we hold to effect change. By standing united in our commitment to ending overdose, supporting those struggling with addiction, and honoring the memory of those we have lost, we can work towards a future where no more lives are needlessly cut short by this devastating epidemic. Together, we can break down the barriers of stigma, offer hope and healing to those who are suffering, and build a society that values compassion, understanding, and the fundamental dignity of every human life.
To learn more, visit www.overdoseday.com.
-
Jumpstarting Your Weight Loss Journey
When it comes to weight loss, some of the most common questions patients will ask are:
“Where do I begin?”
“Should I exercise more?”
“If so, what type of exercise?”
“Should I eat less?”
“If so, what types of foods should I avoid?”In this article you will find answers to all of those questions and more to help get you off to the right start in your weight loss journey.
Food is one of the biggest culprits when it comes to gaining weight. As a result, it’s not uncommon for Canadians to try different types of diets to shed excess pounds. Many of the diets promoted in magazines and on television promise quick and easy weight loss – these are known as “fad” diets. However, these types of diets, unfortunately, do not usually work, which can only lead to feelings of discouragement. With a fad diet, many types of foods are restricted which makes these types of diets much more difficult to follow long-term, and some even limit certain nutrients that the body requires to stay healthy. In order to be successful with weight loss, you need to find a diet plan that works for you and make sure it’s one that you can benefit from – not just for a few days, but also for many months and years to come. This means: Eating healthy, watching portion sizes, and combining it with regular physical activity as well as other lifestyle and habit changes. Yes, weight loss does take some effort and determination, but with the right mindset anything is possible.
In order to build the foundation for success and to be able to maintain a healthy weight over the long-term, you need to:
1. Get motivated. This is key for success. If you’re not in the right frame of mind or aren’t serious about living a healthier life, that’s when you’re more likely to fail. To keep yourself on track you can put little sticky notes around the house reminding you of what you need to do and why (i.e. ‘go to the gym today because I’ll feel better’), or even call up a friend. Sometimes a weight loss journey can be more successful when a partner is involved, as you can hold each other accountable.
2. Uncover the triggers and/or bad habits that led to your weight gain and figure out what you can do to turn those bad habits into healthy ones.
3. Set goals. For some, choosing to live a healthier lifestyle comes easy. For others, they need to see their goals written down on paper in order to be able to fully achieve them. The goals you create can be for both the short and long-term. If you want to lose a certain amount of weight within 2 years, write that down. If you want to start going for more walks around your neighbourhood, write that down. If you want to eat more fruits and vegetables, write that down too. The goals can be as little or as big as you want them to be, as long as they’re your goals and yours only.
When it comes to food, there are also certain things you need to do:
1. In order to stay healthy your body needs food from each of the four food groups listed in Canada’s Food Guide. These four food groups are: Fruits and Vegetables, Grain Products, Milk and Alternatives, and Meat and Alternatives. You should make sure that you are including the minimum number of servings required from these four food groups on a daily basis.
2. Eat three well-balanced meals per day. Breakfast (which is one of the most important meals of the day; you are also less likely to be overweight if you eat breakfast compared to those who skip it), lunch, and dinner.
3. Make sure the foods you eat are also high in fibre. High-fibre foods can help you lose weight as they make you feel full; therefore you’re less likely to overeat. Examples of high-fibre foods include beans, peas, lentils, whole-wheat pasta, nuts and seeds. If you do opt for a high-fibre diet, always make sure you increase water intake to avoid gastrointestinal upset.
4. Avoid junk food. Things like potato chips and cookies are easy to snack on, but they contain little to no nutritional value. If you do happen to get hungry in between meals, switch that junk for something healthy, like fruit or vegetables with low-fat dip and/or Greek yogurt.
5. While a certain amount of fat is needed, you should always choose foods that are lower in fat. The best way to do this is to check out the nutrient facts label on the foods you buy. There, it will list the amount of fat per serving. You should also limit unsaturated fats to just 2 teaspoons per day. Unsaturated fats include any type of fats that you use to cook with, butter, as well as salad dressing, sauces and gravy.
6. Bake foods instead of frying them. Baking foods requires little to no oil, while fried foods often use excessive amounts of oil. Consuming too many fried foods can lead to heart disease and obesity.
Lastly, make sure you’re staying active. You’ll be much more successful in your weight loss journey when you combine healthy eating with regular physical activity (it’s recommended that you get at least 150 minutes of exercise each week/30 minutes per day.) This can be something as simple as mowing the lawn or walking the dog, going for a walk, jogging, bike riding, or joining a gym – as long as it’s something you find enjoyable.